Associations of Migraine and Tension-type Headache with Glaucoma
Article information
Abstract
Purpose
It remains unclear whether primary headaches, particularly migraine, are associated with glaucoma. We investigated potential associations between primary headaches, including migraine and tension-type headache (TTH), and primary glaucoma, including open-angle glaucoma (OAG) and closed-angle glaucoma (CAG).
Methods
We used data from the Clinical Data Warehouse collected between 2008 and 2023 to investigate whether migraine and TTH influence the risk of primary glaucoma. We compared the prevalence of primary glaucoma, including OAG, CAG, other glaucoma, and total glaucoma (TG), among patients with migraine, those with TTH, and controls.
Results
This study analyzed 46,904 patients with migraine, 48,116 patients with TTH, and 455,172 controls. Controls were selected based on propensity score matching (PSM). After adjustment for covariates and PSM, the fully adjusted odds ratios (ORs) for patients with migraine were 1.83 for OAG (95% confidence interval [95% CI], 1.33–2.51; p<0.004) and 1.55 for TG (95% CI, 1.26–1.91; p<0.004) compared to controls. Furthermore, in patients with TTH, the ORs for CAG were 2.20 (95% CI, 1.40–3.47; p<0.004) compared to controls. Additionally, patients with migraine had fully adjusted ORs of 1.71 for OAG (95% CI, 1.24–2.36; p<0.004) and 1.41 for TG (95% CI, 1.15–1.73; p<0.004) compared to those with TTH.
Conclusion
Migraine is associated with primary glaucoma, particularly OAG.
INTRODUCTION
Tension-type headache (TTH) is the most common primary headache disorder, whereas migraine is more debilitating and affects 10-15% of the general population, particularly individuals of working age. Although the pathogenesis of migraine is complex and unclear, several potential mechanisms have been proposed, including vasospasm, hypercoagulability, endothelial, and vascular muscle dysfunction, and vascular changes associated with cortical spreading depression.1-3 Consequently, migraine is considered a systemic vasculopathy.1,4
Glaucoma is a multifactorial disorder characterized by progressive optic neuropathy and visual field loss, which makes it the most common cause of irreversible blindness worldwide.5,6 Primary glaucoma can be categorized as open-angle glaucoma (OAG) or closed-angle glaucoma (CAG), the most common types of glaucoma in Asians.7,8 The pathogenesis of glaucoma involves vascular risk factors. Previous studies have evaluated associations between glaucoma and systemic vascular diseases (e.g., hypertension and diabetes) and ocular vascular factors (e.g., ocular blood flow and perfusion pressure).9-11
A previous study demonstrated a slightly increased risk of CAG in individuals with hyperlipidemia, liver diseases, peptic ulcers, and headaches. Furthermore, in a previous study, headache, but not migraine, was associated with a higher risk for CAG.12 Recent epidemiological studies have demonstrated an association between migraine and OAG, revealing that individuals with migraine are more likely to develop OAG than those without migraine, even after adjusting for risk factors.13,14 Conversely, another study of Chinese individuals revealed that migraine did not increase the risk of OAG.15 Therefore, it remains unclear whether primary headaches, particularly migraine, are concomitant conditions or risk factors for glaucoma.
Here we investigated the relationships between primary glaucoma, including OAG and CAG, and migraine and TTH, the main types of primary headache.
MATERIALS AND METHODS
1. Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Clinical Research Ethics Committee of Chuncheon Sacred Heart Hospital, Hallym University (No. 2024-01-001). Because this study used only deidentified data, the review board waived the requirement for obtaining informed consent form all subjects.
2. Study participants
We analyzed clinical data from the Smart Clinical Data Warehouse (CDW), Hallym University Medical Center, collected between January 2008 and November 2023. The Smart CDW, based on the Qlik-View Elite Solution (Qlik), is used at all five Hallym University Medical Center hospitals. It enables the extraction and integrated analysis of fixed data from electronic medical records. Patients with migraine were eligible for inclusion in this study if they were aged 20-80 years, were diagnosed by a board-certified neurologist, were assigned the International Classification of Diseases tenth revision (ICD-10) code G43 in medical records, and had more than two outpatient visits or at least one admission to a neurology department. Patients with TTH were included if they were aged 20-80 years and assigned the ICD-10 code G44 in the database. The control group included patients aged 20-80 years who had undergone general health checkups at a health promotion center. Patients with a history of headache or migraine identified using a basic questionnaire administered before the health checkup were excluded.
3. Migraine, tension-type headache, glaucoma, and covariates
We compared the frequency of primary total glaucoma (TG), excluding secondary causes, among patients with migraine, TTH, and controls. Glaucoma was diagnosed based on the ICD codes in the CDW database. We excluded secondary cases using ICD codes (H40.3-6). In addition, primary glaucoma was classified as OAG (H40.1), CAG (H40.2), and other glaucoma (OG; H40.8-9). In addition, the presence of comorbidities was determined using relevant ICD-10 codes in the database, including angina (I20, I24, and I251), atrial fibrillation (I480–482 and I489), anxiety disorder (F41), cerebrovascular diseases (G45-46 and I60-69), chronic hepatitis (B18, I85, and K70-74), chronic pulmonary disease (J44), depression (F31-34, F412, and F432), diabetes mellitus (E10-14), dyslipidemia (E78), heart disease (I05-09, I21-23, I30-47, and I49-52), hypertension (I10-15), menopause (M800, M010, N924, and N95), renal failure (N03 and N18-17), and sleep disorders (F51, G258, and G47). We excluded patients with renal failure receiving concurrent dialysis prescriptions to exclude dialysis headaches.
4. Statistical analysis
Continuous data are presented as means with standard deviations, whereas categorical data are presented as frequencies with percentages. The T-test and chi-square test were used to compare continuous and categorical data among migraine, TTH, and control groups. Given the inability to randomize patients based on migraine or TTH status, we used propensity score matching (PSM) to adjust for covariates and selection bias using Python (version 3.7; Anaconda Inc.; https://www.anaconda.com) and Pymatch (version 0.3.4; https://github.com/benmiroglio/pymatch). Propensity scores ranged from 0.07 to 0.87; all matched cases had scores within 0.0001 of each other at a matching ratio of 1:1. This process resulted in 14,177 matched pairs of migraine patients and controls, 20,325 matched pairs of TTH patients and controls, and 12,808 matched pairs of migraine and TTH patients. Logistic regression was used to calculate odds ratios (ORs) with 95% confidence intervals (CIs) for outcomes in the OAG, CAG, OG, and TG groups compared to their respective controls. After PSM, adjusted ORs were computed for each disorder among the three groups using covariates and propensity scores. The Bonferroni correction was applied to correct for multiple testing and p-values<0.004 were considered significant. This value was derived by dividing the p-value threshold of 0.05 by the number of tests performed, i.e., 12 (four outcome variables tested in three groups). All p-values were two-sided. SPSS software (version 24.0; IBM Corp.) was used for statistical analyses.
RESULTS
1. Participant characteristics
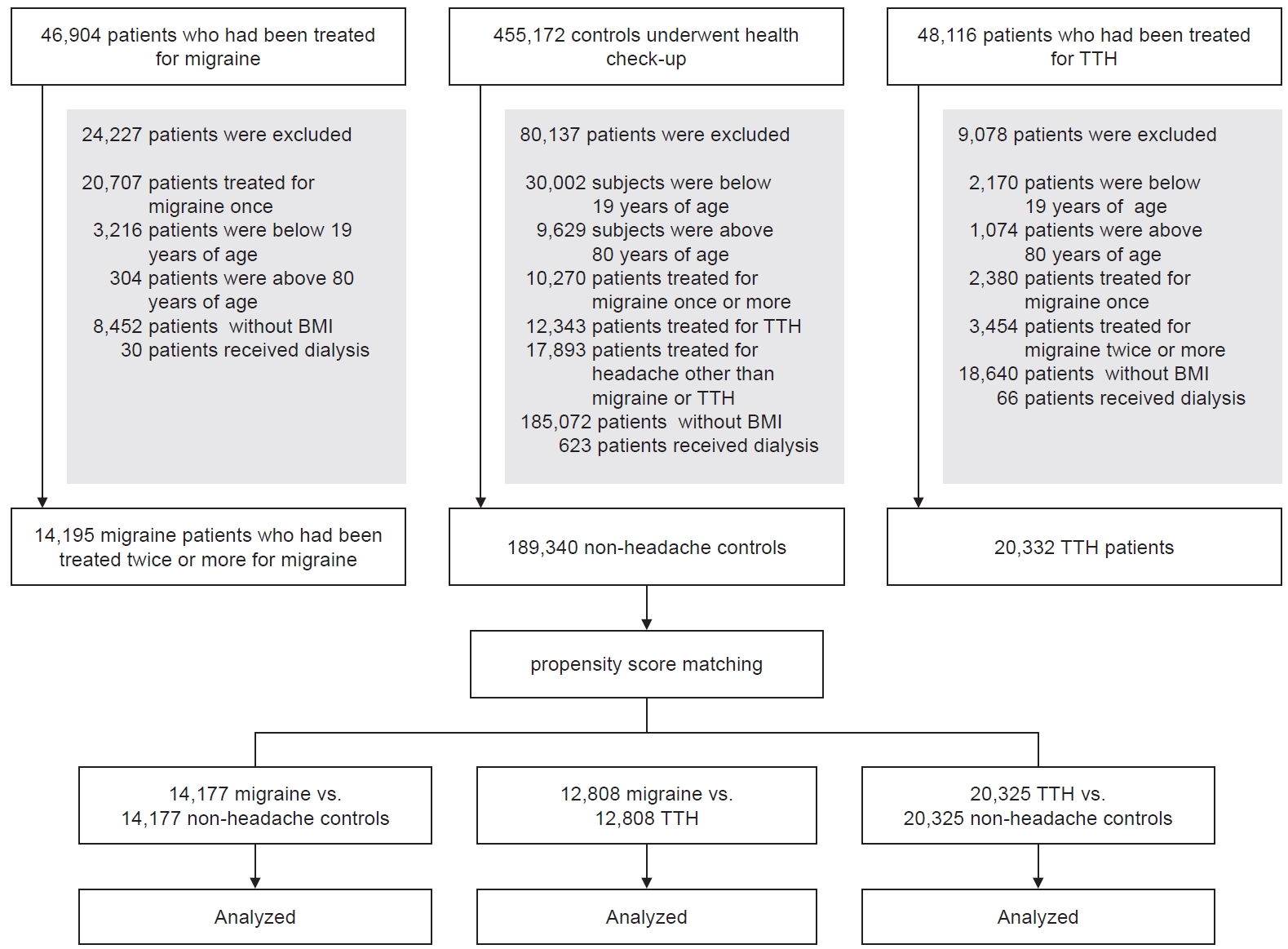
In total, 46,904 patients with migraine, 48,116 patients with TTH, and 455,172 controls were enrolled using the ICD-10 codes. After the application of exclusion criteria, 14,195 migraine patients, 20,332 TTH patients, and 189,340 controls were included in the final analysis. Of the enrolled patients with migraine, 10,523 were females (74.1%) and the mean age was 45.6±14.4 years. In the TTH and control groups, 12,344 (60.7%) and 91,309 participants (48.2%) were females; the mean ages were 52.8±13.7 and 49.8±14.7 years, respectively. Figure 1 presents the enrollment process. After PSM, absolute standardized differences between the migraine and control groups were <0.1 (Table 1). Furthermore, no significant differences were observed between the TTH and control groups (Table 2). After PSM, no significant differences were observed between the migraine and TTH groups (Table 3).
2. Primary glaucoma in patients with migraine and controls
Prior to PSM, unadjusted ORs in individuals with migraine compared to controls were 1.74 (95% CI, 1.27-2.39; p<0.004) for OAG, 2.30 (95% CI, 1.10-4.84) for CAG, 1.03 (95% CI, 0.80-1.33) for OG, and 1.46 (95% CI, 1.19-1.79; p<0.004) for TG. After PSM, the adjusted ORs were 1.83 (95% CI, 1.33-2.51; p<0.004) for OAG, 2.55 (95% CI, 1.21-5.39) for CAG, 1.10 (95% CI, 0.85-1.43) for OG, and 1.55 (95% CI, 1.26-1.91; p<0.004) for TG in migraine patients (Table 4). Among all types of primary glaucoma, only OAG was associated with migraine.
3. Primary glaucoma in patients with tension-type headache and controls
Table 5 presents the ORs for the development of primary glaucoma in TTH patients and controls. The unadjusted ORs for OAG, CAG, OG, and TG were 1.46, 2.07, 1.02, and 1.20 in TTH patients compared to controls, respectively. After adjusting for all covariates and PSM, the fully adjusted ORs in patients with TTH compared to controls were 1.53 (95% CI, 1.18-1.98) for OAG, 2.20 (95% CI, 1.40-3.47; p<0.004) for CAG, 1.08 (95% CI, 0.89-1.30) for OG, and 1.27 (95% CI, 1.08-1.48) for TG (Table 5). Among all types of primary glaucoma, only CAG was associated with TTH patients.
4. Differences in primary glaucoma between patients with migraine and tension-type headache
A comparison of patients with migraine and TTH demonstrated fully adjusted ORs of 1.71 (95% CI, 1.24-2.36; p<0.004) for OAG, 1.12 (95% CI, 0.62-2.03) for CAG, 1.19 (95% CI, 0.91-1.56) for OG, and 1.41 (95% CI, 1.15-1.73; p<0.004) for TG. Among all types of primary glaucoma, only OAG was associated with migraine (Table 6).
DISCUSSION
We investigated the risk of primary glaucoma, including each major type, among patients with migraine and TTH based on CDW data collected between 2008 and 2023. After adjusting for covariates and employing PSM, patients with migraine were at a significantly higher risk of OAG, whereas patients with TTH were at a higher risk of CAG, compared to controls without headache. Moreover, migraine was associated with a higher risk of primary glaucoma, particularly OAG, compared to TTH. Therefore, migraine may be considered a potential contributing factor for OAG.
It remains unclear whether migraine significantly increases the risk of OAG. Previous studies have demonstrated that individuals with migraine have a higher risk of developing OAG compared to those without migraine.14 In one study, the association between OAG and migraine was significant only for individuals aged 70-79 years and those aged <50 years with no comorbidities.16,17 Conversely, other studies have revealed that migraine does not increase the risk of OAG15,18,19 or CAG.15 Furthermore, in another study, no significant association was found between migraine and OAG after adjusting for confounding variables.19
Our retrospective study demonstrated a significantly higher prevalence of glaucoma in migraine patients than controls and TTH patients. Although the comparison with the headache-free control group aligns with previous studies, the comparison between the TTH and migraine groups was considered meaningful due to the divergence from previous studies. A meta-analysis suggested that migraine may significantly increase the risk of developing OAG.20 However, some cohort studies have failed to confirm this association. As a result, it remains unclear whether migraine increases the risk of OAG.
Glaucoma is characterized by progressive degeneration of retinal ganglion cells and optic nerve axons. Based on pathophysiological and anatomical features, glaucoma is categorized into OAG and CAG. The pathogenesis of glaucoma involves factors such as oxidative stress, excitotoxicity, altered immunity, and impaired microcirculation.21 Although the exact pathophysiology of migraine is unclear, it is associated with neurovascular dysfunction resulting from vascular changes, impaired hypoperfusion, and microembolism.22 Several epidemiological studies have demonstrated the role of vascular risk factors in the pathogenesis and progression of glaucomatous optic neuropathy.11,16,23-27 A pooled analysis of the associations between systemic vascular risk factors and OAG revealed that hypertension is the most significant risk factor for OAG. However, the relationships between OAG, type 2 diabetes mellitus, and migraine require further evaluation.11
In the present study, patients with TTH had a higher risk of CAG compared to controls. Furthermore, migraine was associated with primary glaucoma, particular OAG, compared to TTH. A population-based retrospective cohort study based on the Taiwan Health Insurance Database revealed that headaches were associated with a 1.13-fold higher risk of CAG; however, there was no significant association between migraine and CAG.12 Patients with CAG can experience headache due to increased intraocular pressure, which may lead to a diagnosis of CAG. CAG should be considered among individuals older than 40 years with late-onset headaches.28,29 TTH is the most common type of primary headache and has non-characteristic features, which may explain the high prevalence of CAG in patients with TTH. Further studies are needed to explore the associations between primary headaches other than migraine and glaucoma.
Our study had several limitations. First, the retrospective collection of clinical data from individuals presenting to a university medical center with five affiliated hospitals may limit the generalizability of our results. Therefore, we cannot establish a causal relationship, and the possibility of an inverse correlation cannot be ruled out. Second, we did not account for potential sources of selection bias and confounding variables. Third, our retrospective design did not allow for the collection of clinical data on headache characteristics (e.g., frequency) or medication history (e.g., triptan use). In addition, the diagnoses of glaucoma, and other comorbid diseases were determined based on the ICD codes recorded in the CDW database. Thus, detailed clinical information regarding glaucoma was not collected. Future prospective, population-based studies are needed to investigate the association between primary headaches and glaucoma.
In conclusion, our analysis of CDW database data revealed a significant association between migraine and OAG, whereas TTH was significantly associated with CAG, compared to controls without headache. Moreover, a significant association was observed between migraine and primary glaucoma, particularly OAG, compared to TTH. Future prospective studies are needed to fully investigate the associations of glaucoma with migraine and TTH.
Notes
Availability of data and material
The data presented in this study are available upon reasonable request from the corresponding author.
Author contributions
Conceptualization: SHL, JHS; Data curation: JHK, YSK; Formal analysis: JHK; Investigation: JHK, JHS; Methodology: JHK, JHS; Software: JHK, JHS; Validation: JHK, JHS; Writing–original draft: JHK, JHS; Writing–review and editing: all authors.
All authors have read and agreed to the published version of the manuscript.
Conflict of interest
Jong-Hee Sohn is the Editor of Headache and Pain Research and was not involved in the review process of this article. All authors have no other conflicts of interest to declare.
Funding statement
This research was supported by “Physician scientist training and future medical technology implementation for solving clinical challenges in nervous system” (RS-2023-00223501). The role of funding was in the design of the study and collection, analysis, and interpretation of data. No other financial relationships relevant to this publication were disclosed.
Acknowledgments
Not applicable.