What a Neurologist Should Know about Functional Anatomy for Botulinum Toxin Injections in the Head, Face, and Neck: A Practical Perspective
Article information
Abstract
Since botulinum toxin (BoNT) was approved by the US Food and Drug Administration as a prophylactic treatment for chronic migraines in 2010, subsequent studies have shown that BoNT is effective in the management of chronic migraines due to its pain-relieving effects. Therefore, neurologists are increasingly utilizing BoNT as a therapeutic tool for chronic migraine. It is crucial to thoroughly understand the functional anatomy in the head, face, and neck regions to successfully administer BoNT injections in these areas. This review describes the complexity of muscles and their associated target nerves in the frontal, temporal, and occipital areas and serves as a resource for essential functional anatomy, with the goal of providing clinicians with a practical perspective on utilizing BoNT injections.
INTRODUCTION
Botulinum toxin (BoNT) is among the treatments approved by the US Food and Drug Administration for the prevention of headaches in patients with chronic migraine (CM).1 The multifaceted mechanisms underlying the analgesic properties of BoNT have been elucidated in the medical literature. In addition to its well-established role in inhibiting acetylcholine release at the neuromuscular junction,2 BoNT influences sensory neurons and neurotransmitter release, thus modulating pain signaling pathways.3,4 The mechanism of action of BoNT in treating pain is most likely related to the inhibition of nociceptive mediator release from afferent neurons, thereby attenuating peripheral pain signaling to the brain.5 A significant aspect of BoNT’s mechanism of action involves its interaction with calcitonin gene-related peptide (CGRP), implicated in the pathophysiology of CM. CGRP is known to play a crucial role in mediating neurogenic inflammation and pain transmission within the trigeminovascular system.6 Studies have shown that BoNT attenuates CGRP release from trigeminal neurons, disrupting the nociceptive cascade associated with migraine attacks.7,8 Moreover, BoNT regulates the expression and function of various neurotransmitters and receptors involved in pain perception, including glutamate, substance P, and transient receptor potential channels.6,9 Furthermore, BoNT’s ability to suppress the release of pro-inflammatory cytokines and alleviate neurogenic inflammation contributes to its anti-nociceptive properties.8,10
The use of BoNT for preventive migraine treatment has been well studied. Data from the Phase Ⅲ Research Evaluating Migraine Prophylaxis Therapy (PREEMPT) trial showed a 50% reduction in headache frequency at all time points compared with placebo-treated patients and patients reported an improvement in health-related quality of life.1,11,12 Based on the PREEMPT trials, BoNT is an effective as a management tool for CM and is well tolerated when the injections follow the PREEMPT guidelines even the injection technique is very complicated and equivocal.13
Despite the recent anatomical studies demonstrating the locations of muscles and nerves over the recent years,14-20 there are only a few functional anatomical studies for BoNT injection in the head, face, and neck. In this review, we try to provide a practical perspective for the BoNT injection technique based on not only the muscles but also the target nerves and their anatomical relationships.
THE FUNCTIONAL ANATOMY OF NERVES AND MUSCLES INVOLVED IN HEADACHES21
1. Frontal area
1) Supratrochlear nerve and corrugator supercilii muscle
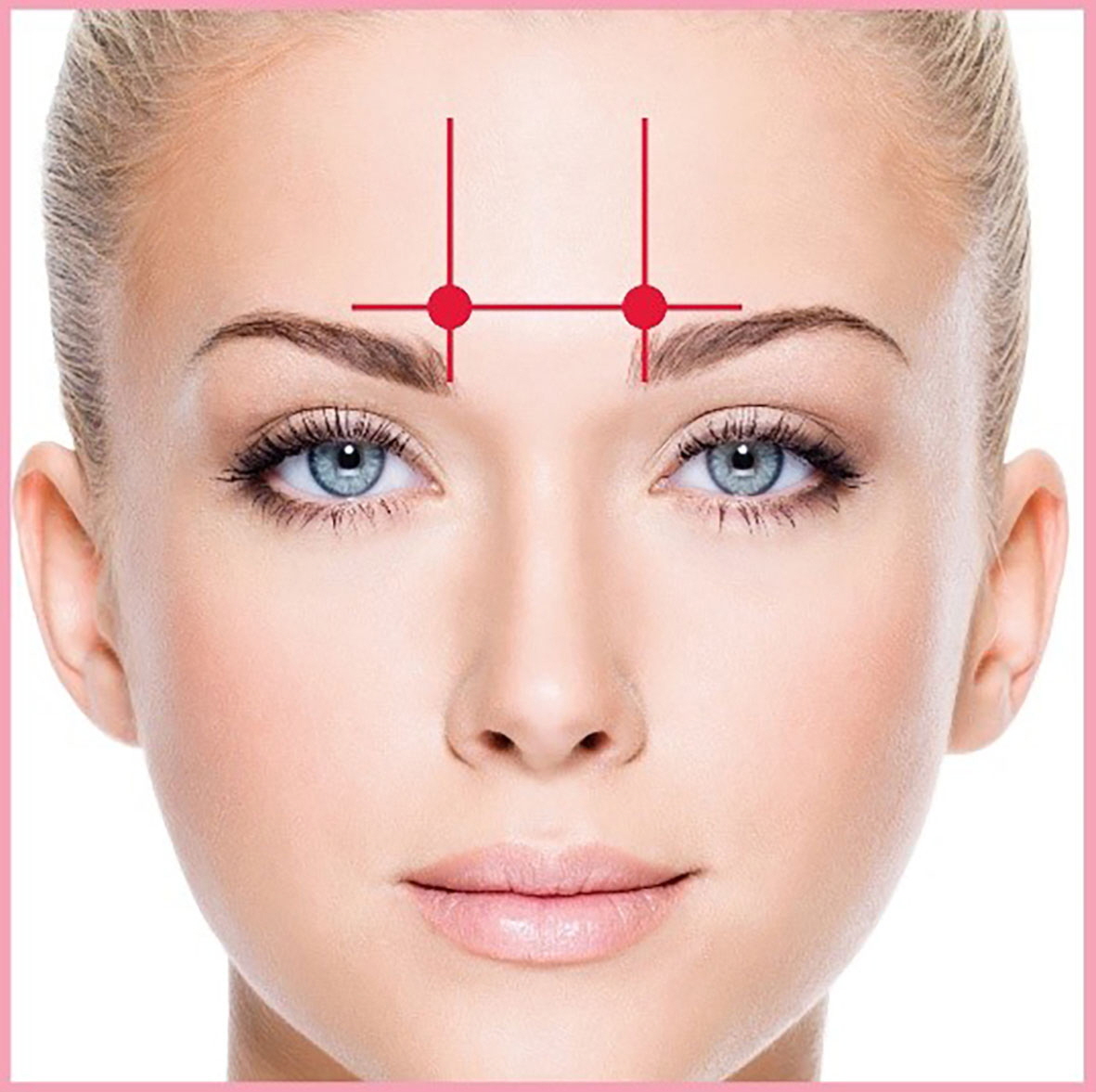
The supratrochlear nerve (STN) is one of the terminal branches of the frontal nerve, a major branch of the ophthalmic nerve. It travels over the roof of the orbit anteromedially, passing through the corrugator supercilii muscle (CSM), and proceeds to the frontal belly of the occipitofrontalis muscle to provide sensation to the mucosa of the glabella, upper eyelid, and skin of the lower forehead close to the midsagittal line (Figure 1).22
Distributions of the supratrochlear nerve (STN), supraorbital nerve (SON), and corrugator supercilii muscle (CSM). A previous study measured the point where the SON entered the CSM and the distance between the SON and the STN. The entry point of the STN into the CSM was found to be 16.4±4.0 mm lateral to the midsagittal line and 2.3±3.9 mm superior to the supraorbital margin. When the STN emerged separately from the orbit, it was situated 7.5±2.3 mm medial to the SON at the level of the supraorbital margin.24 Chronic migraines can be relieved by injecting botulinum toxin at the location indicated by the blue dot.
VL, vertical baseline; HL, horizontal baseline.
The relationship between the STN and the CSM is clinically significant, especially in the context of CMs. Some opinions suggest that CMs have been associated with the entrapment of the STN within the CSM.23-25 Possibly due to hyperactivity of the muscle, entrapment or compression of the STN by the CSM can be a trigger point for headaches in the frontal region.24,25 BoNT injections in the frontal region aim to alleviate migraine symptoms by targeting the STN and relaxing the CSM, potentially relieving to nerve entrapment.24
(1) Corrugator muscle injection
‣ The proper BoNT dilution for CM is 2 mL of saline per 100 U. The resulting concentration is 5 U per 0.1 mL.
‣ DOSE: One injection of 0.1 mL on the left and right sides (a total of two injections)
‣ The corrugator muscle injection site is located one finger’s breadth (1.5 cm) above the medial superior edge of the orbital ridge (bony landmark).
‣ Inject with the needle pointing upward at a 45-degree angle away from the medial aspect of the muscle to avoid ptosis of the eyelid (Figure 2).26
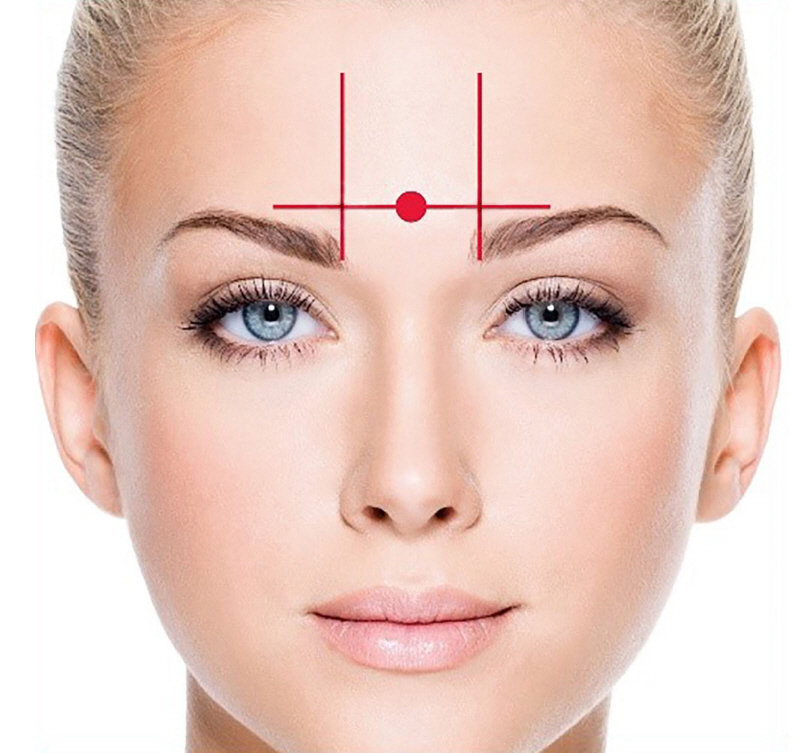
(2) Procerus muscle injection
‣ The procerus muscle injection site is midline on the forehead, approximately one finger’s breadth (1.5 cm) above and midline to the medial superior aspect of each eye's orbital ridge (bony landmark).
‣ The injection site for this muscle should be approximately midway between the two corrugator injections (visualize a single straight line connecting all three of these injections).
‣ Inject with the bevel of the needle pointing upward (Figure 3).26
2) Supraorbital nerve and frontalis muscle
The supraorbital nerve (SON) is a branch of the frontal nerve, a branch of the ophthalmic division of the trigeminal nerve (cranial nerve V). It emerges from the supraorbital foramen (or notch) and innervates the skin of the forehead, scalp up to the vertex, and the upper eyelid (Figure 1).27
The relationship between the SON and the frontalis muscle is primarily anatomical and functional within the context of the forehead’s sensory and motor activities. Emerging from the supraorbital foramen, the SON provides sensory innervation to the forehead skin, which overlays the frontalis muscle. This innervation includes touch, pain, and temperature sensations within the frontalis muscle's region.
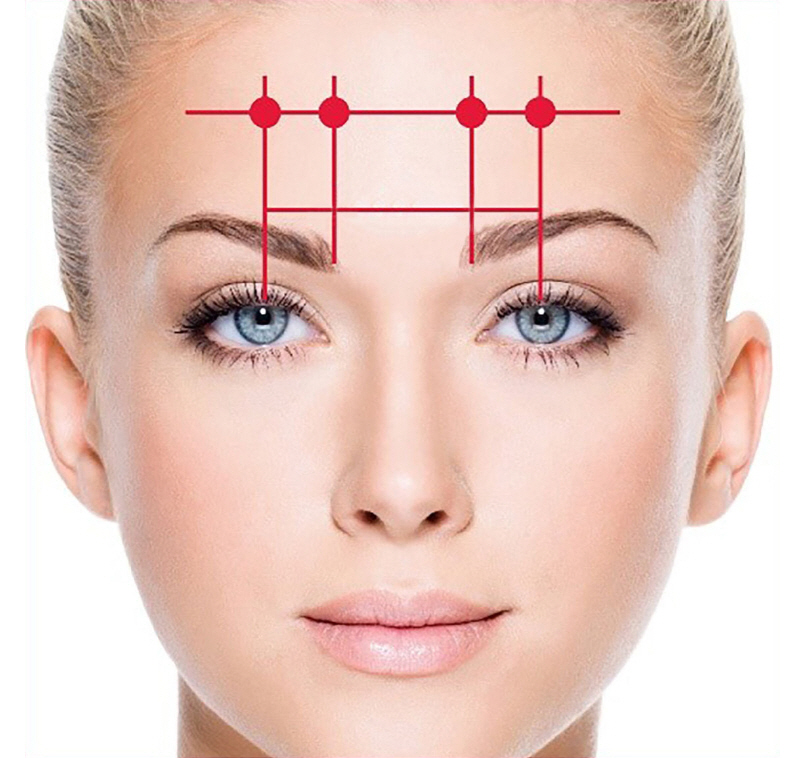
(1) Frontalis muscle injection
‣ The proper BoNT dilution for CM is 2 mL of saline per 100 U. The resulting concentration is 5 U per 0.1 mL.
‣ DOSE: Two injections of 0.1 mL on the left and right sides (a total of four injections) (Figure 4)26
‣ Make sure the needle stays superficial to avoid the periosteum. A good rule of thumb is to inject superficially enough to raise a bleb.
Medial injection sites:
‣ Visually, draw a line up from the medial edge of the eyebrow.
‣ The injection site is about one finger’s breadth (at least 1.5 cm) above the corrugator injection site.
Lateral injection sites:
‣ The injection sites are parallel and about one finger’s breadth (at least 1.5 cm) lateral to the first two injection sites. This may vary based on individual anatomy.
It has been reported that 5 U each of BoNT-A should be injected in four sites of the frontalis muscle. The medial injection sites are located at a point with an invisible line drawn up at least 1.5 cm (≈ one finger’s breadth) from the medial end of the eyebrow from the corrugator injection site. The lateral injection sites are at least 1.5 cm (≈ one finger’s breadth) lateral and parallel to the medial injections sites explained previously. When BoNT-A is injected to treat CM, an unexpected clinical side effect may occur. The “Mephisto sign” may develop as a side effect of BoNT-A injection into the frontalis muscle, whereby the outer end of the eyebrow is located above the inner end, possibly producing an intimidating impression (Figure 5).26
Mephisto sign development. (A) Before botulinum toxin A (BoNT-A) injection: photograph of the patient’s frontal view before BoNT-A injection, showing normal eyebrow alignment. (B) Two weeks after the BoNT-A injection: photograph of the same patient’s frontal view two weeks after the BoNT-A injection, demonstrating the development of the Mephisto sign, characterized by the outer end of the eyebrow positioned higher than the inner end, potentially creating an intimidating impression. Adapted from the book of Kim ST et al. (Dental Wisdom; 2018) with permission of copyright holder.26
A previous study proposed that the development of the Mephisto sign may be prevented with an additional BoNT-A injection of 2–4 U bilaterally to the lateral most point of the frontalis muscles during the primary injection process.28
2. Temporal area
1) Auriculotemporal nerve and temporalis muscle
The auriculotemporal nerve (ATN) is a branch of the mandibular nerve, a part of the trigeminal nerve (cranial nerve V). It emerges in the facial region, specifically passing by the temporomandibular joint area by the area of the temporomandibular joint and extending into the temple region of the scalp. The ATN provides sensory innervation to the tragus, the anterior portion of the ear, and the temple region. Anatomical studies have highlighted the ATN’s significant relationship with the superficial temporal artery, with variations in their interaction potentially contributing to migraine pathophysiology. Specifically, in some individuals, the ATN and the superficial temporal artery run closely together or even intertwine, which may act as a peripheral trigger point for migraines.29
This anatomical layout emphasizes the ATN’s superficial course over the temporalis muscle, which becomes a critical consideration in administering BTX-A injections for migraine management. The superficial course of the ATN over the temporalis muscle guides the subcutaneous administration of BTX-A, aiming to maximize the therapeutic effects by targeting the nerve pathways directly involved in migraine pathophysiology (Figure 6).26,30
2) Zygomaticotemporal nerve and temporalis muscle
The zygomaticotemporal nerve (ZTN) is a branch of the maxillary division of the trigeminal nerve. In relation to the temporalis muscle, the ZTN leaves the lateral zygoma to enter the temporal fossa and ascends through the temporalis muscle or between this muscle and its outer fascia to become subcutaneous near the pterion. It primarily distributes to the skin of the anterior temporal region.31
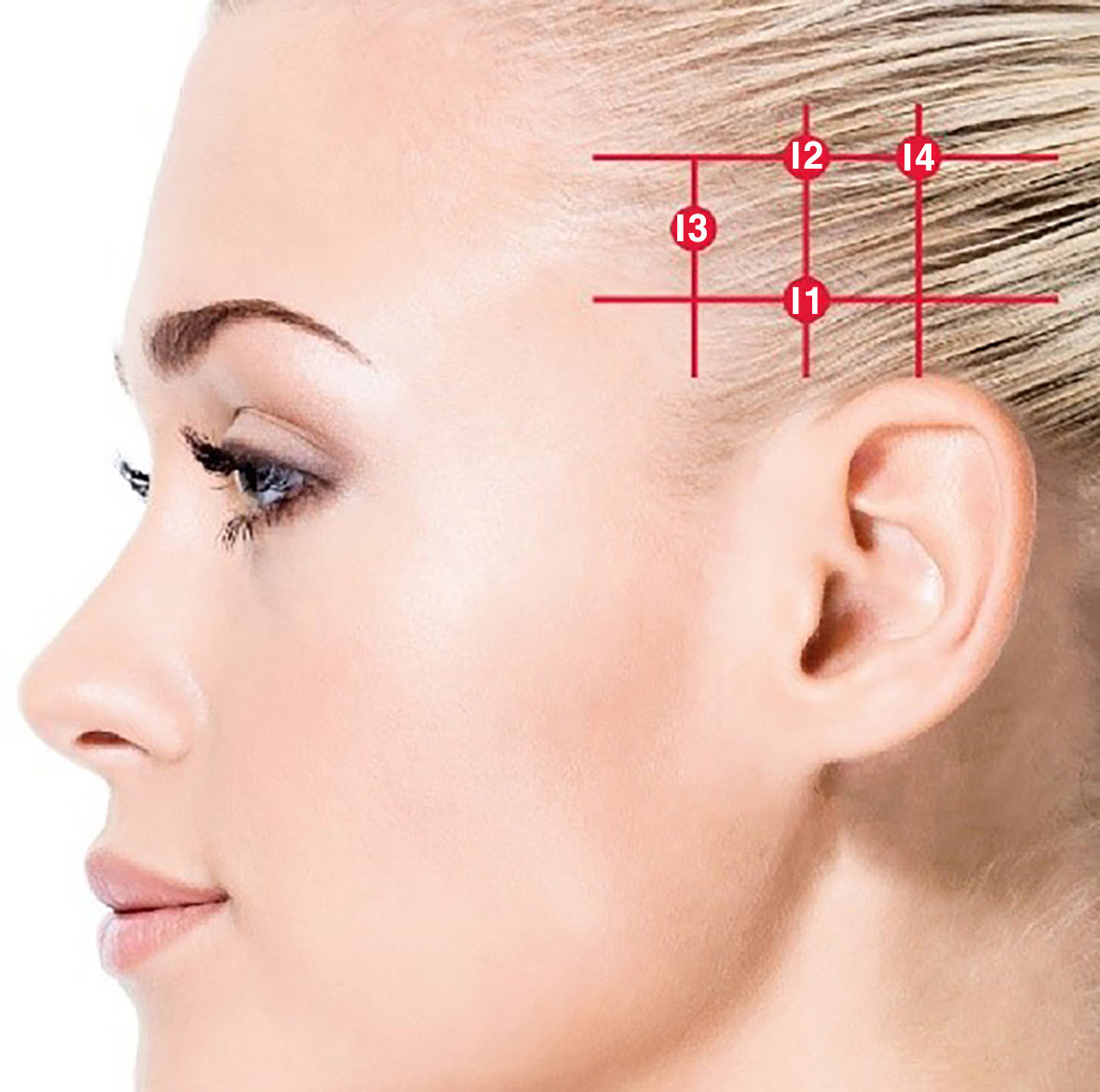
(1) Temporalis muscle injection (fixed-site, fixed-dose)
A proposal for BoNT type A injection into the temporal region in CM headache
‣ The proper BoNT dilution for CM is 2 mL of saline per 100 U. The resulting concentration is 5 U per 0.1 mL.
‣ FIXED-DOSE INJECTIONS: Four injections of 0.1 mL on the left and right sides (a total of eight injections)
‣ Begin with the left temporalis muscle (i.e., fixed-dose injections first, followed by any follow-the-pain injections). Repeat the procedure symmetrically on the right side.
Injection 1:
‣ Locate the tragus of the ear and move your finger vertically upwards along the side of the head approximately two finger’s breadth (3 cm).
Injection 2:
‣ Proceed approximately 1.5 to 3 cm upwards from the point of Injection 1, still in line with the tragus of the ear.
Injection 3:
‣ Move forward towards the face approximately one to two finger’s breadth (1.5 to 3 cm) from the locations of the first and second injections. Make the third injection midway between injection sites one and one along the vertical axis.
‣ Retreat approximately one finger’s breadth (1.5 cm) behind the point of Injection 2, aligning with the midpoint of the ear.
3. Occipital area
1) Great occipital nerve and occipital muscle
The great occipital nerve (GON) is the largest of the three occipital nerves, originating as the medial branch of the posterior (dorsal) ramus of the C2 spinal nerve. The GON also provides communicating branches that anastomose with the lesser and third occipital nerves (TONs).
The GON is closely related to the occipital muscles, specifically the semispinalis capitis muscle. This anatomical relationship is significant because the pathway of the GON through these muscles is a potential site for nerve entrapment or irritation, which can contribute to conditions like occipital neuralgia (Figure 8).19,32
The great occipital nerve (GON, yellow line) is located at the third point of the virtual line, connecting the external occipital protuberance (inion) and the mastoid process (white dots). The injection sites are as follows: at the midpoint(<-middle point) of the virtual line connecting the mastoid process and inion, a point in the shape of an inverted triangle set around 3 cm from the first site and two other points that constitute the vertices of the inverted triangle. Finally, botulinum toxin (BoNT) was injected into three points (red dots) around GON, where 5 U of BoNT was administered at each point.32
(1) Occipitalis muscle injection (fixed-site, fixed-dose)
‣ The proper BoNT dilution for CM is 2 mL of saline per 100 U. The resulting concentration is 5 U per 0.1 mL.
‣ FIXED-DOSE INJECTIONS: Three injections of 0.1 mL on the left and right sides (a total of six injections)
‣ To locate the occipitalis injection sites, palpate for the external occipital protuberance.
‣ Stay superior to the supranuchal ridge on either side of the occipital protuberance.
‣ Begin with the left occipitalis muscle (i.e., fixed-dose injections first, followed by any follow-the-pain injections). Repeat the procedure symmetrically on the right side.
Injection 1:
‣ Position your thumb at the midpoint of the occipital protuberance and your index finger at the tip of the mastoid process. Divide the space between them in half and administer the first injection just above the nuchal ridge at this midpoint.
Injection 2:
‣ Measure a diagonal fingerbreadth up and out toward the superior helix of the ear for the second injection site.
Injection 3:
‣ Measure a diagonal fingerbreadth up and medial for the third muscle area for injection (Figure 9).32
2) Third occipital nerve and cervical paraspinals muscle
The TON, also known as the least occipital nerve, originates from the posterior (dorsal) ramus of the C3 spinal nerve. The relationship between the TON and the cervical paraspinalis muscles becomes clinically relevant in conditions like occipital neuralgia or chronic headaches, where muscle tension in the cervical region can contribute to nerve irritation or entrapment, leading to pain syndromes. Although the pilot study on BoNT treatment focuses on the GON and its efficacy in treating chronic occipital neuralgia, the principles of muscle-nerve interactions can also apply to the TON.33
(1) Cervical paraspinals muscle injection
‣ The proper BoNT dilution for CM is 2 mL of saline per 100 U. The resulting concentration is 5 U per 0.1 mL.
‣ DOSE: Two injections of 0.1 mL on the left and right sides (a total of four injections)
‣ To locate the cervical paraspinal muscle group injection sites, palpate the cervical spine.
‣ Begin with the left cervical paraspinal muscle. Repeat the procedure symmetrically on the right side.
Injection 1:
‣ The first injection should be 1 cm left of the midline of the cervical spinal muscle and ~3 to 5 cm inferior to the occipital protuberance.
Injection 2:
‣ This should be 1 cm superior diagonally toward the ear from the first injection (Figure 10).26

Cervical paraspinal muscle injection. Adapted from the book of Kim ST et al. (Dental Wisdom; 2018) with permission of copyright holder.26
CONCLUSIONS
The revealed analgesic effects of BoNT have garnered considerable interest among neurologists, as it can be used as an effective prophylactic treatment for CMs. The multifaceted content presented in this review underscores the importance for clinicians to comprehend the anatomical complexity between muscles and target nerves in the frontal, temporal, and occipital regions to ensure precise administration of BoNT injections. In particular, it elucidates the anatomical relationships between muscles and nerves in the frontal region, including STN, CSM, SON, and frontalis muscle, as well as in the temporal region, encompassing ATN, ZTN, and temporalis muscle, and in the occipital region, involving GON, occipital muscles, TON, and cervical paraspinalis muscles. Consequently, it emphasizes the significance of considering both muscles and nerves in BoNT injection techniques.
The objective of this perspective is to provide clinicians with a comprehensive resource on BoNT injection sites and techniques, facilitating the successful administration of BoNT injections for the management of CM. As neurologists increasingly embrace BoNT as a therapeutic tool, the goal is for clinicians to deepen their understanding of functional anatomy, utilizing it as a therapeutic modality to contribute to improved patient outcomes in the realm of CM treatment.
Notes
AVAILABILITY OF DATA AND MATERIAL
All data generated or analyzed during this study are included in this published article.
AUTHOR CONTRIBUTIONS
Conceptualization: VF, STK; Data curation: SRK, STK; Formal analysis: AHK, STK; Investigation: AHK, STK; Methodology: AHK, STK; Writing–original draft: SRK, STK; Writing–review & editing: SRK, VF, AHK, STK.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING STATEMENT
Not applicable.
ACKNOWLEDGMENTS
Not applicable.