Abstract
- This case report presents pathological findings in a rare case of cerebral venous thrombosis (CVT) caused by spontaneous intracranial hypotension (SIH) that was treated successfully with mechanical thrombectomy. The etiologies and prognosis of CVT vary, and CVT resulting from SIH is particularly uncommon and challenging to diagnose and manage. In this case, magnetic resonance imaging revealed signs consistent with both SIH and CVT, which contributed to the patient’s worsening weakness. The patient was treated with a combination of endovascular thrombectomy and epidural blood patch, followed by anticoagulation therapy, and recovered without any complications. A pathological analysis of the retrieved thrombus using hematoxylin and eosin staining showed a high proportion of fibrin and platelets, which could shed light on the mechanism of CVT induced by SIH under conditions of low blood flow due to venous engorgement.
-
Keywords: Intracranial hypotension, Thrombectomy, Venous thrombosis
INTRODUCTION
Spontaneous intracranial hypotension (SIH) is an uncommon condition characterized by a decrease in intracranial pressure due to cerebrospinal fluid (CSF) leakage, occurring without any history of procedures or trauma that could cause dural defects.1 Patients typically present with orthostatic headache, which worsens in the upright position and improves when lying down.2 Other neurological symptoms include nausea, neck pain, vomiting, neck stiffness, anorexia, diaphoresis, diplopia, photophobia, hiccups, unsteady gait, hyperacusis, tinnitus, blurred vision, and altered mentality.2,3 However, in some cases, the effects of SIH extend beyond these symptoms to severe neurological complication such as cranial nerve palsy, subdural hemorrhage, subdural effusion, and cerebral venous thrombosis (CVT).3-6
In the past decade, there have been numerous reports of CVT associated with SIH, with an estimated incidence of 1%–2% among SIH patients.6 The mechanism by which SIH leads to CVT remains unclear, but it is hypothesized to involve compensatory dilation of the cerebral venous system according to the Monro-Kellie doctrine, damage to the venous walls due to changes in cerebral buoyancy, and increased viscosity of venous blood.7
Anticoagulant therapy is generally used for CVT, however, there is no consensus on its use for CVT secondary to SIH.7-9 The authors report a case of a 43-year-old woman who presented with progressive limb weakness following an orthostatic headache. SIH complicated by CVT was identified, and the patient showed improvement after undergoing endovascular thrombectomy and epidural blood patch, followed by anticoagulation therapy. We also present the histological analysis results of the retrieved thrombus, which could shed the light of mechanism of CVT induced by SIH.
CASE REPORT
1. Ethics approval and consent to participate
This study was approved by the Institutional Review Board (IRB) of the Ewha Womans University Seoul Hospital (No. 2023-11-030) and informed consent was obtained.
2. Case
A 43-year-old woman experienced a gradual worsening of occipital and posterior neck pain accompanied by nausea. From the onset, her symptoms were orthostatic and almost completely relieved by lying down, but progressively worsened over the past 2 weeks. One morning, she suddenly woke up with a thunderclap headache (numeric rating scale 10) that did not improve when lying down, and felt weakness in her left upper and lower extremities, prompting a visit to our hospital. In the emergency room, she presented with numbness on the left side of her face and body, dysarthria, and motor weakness in four extremities, classified as motor grade II, with worsening neurological symptoms than at home.
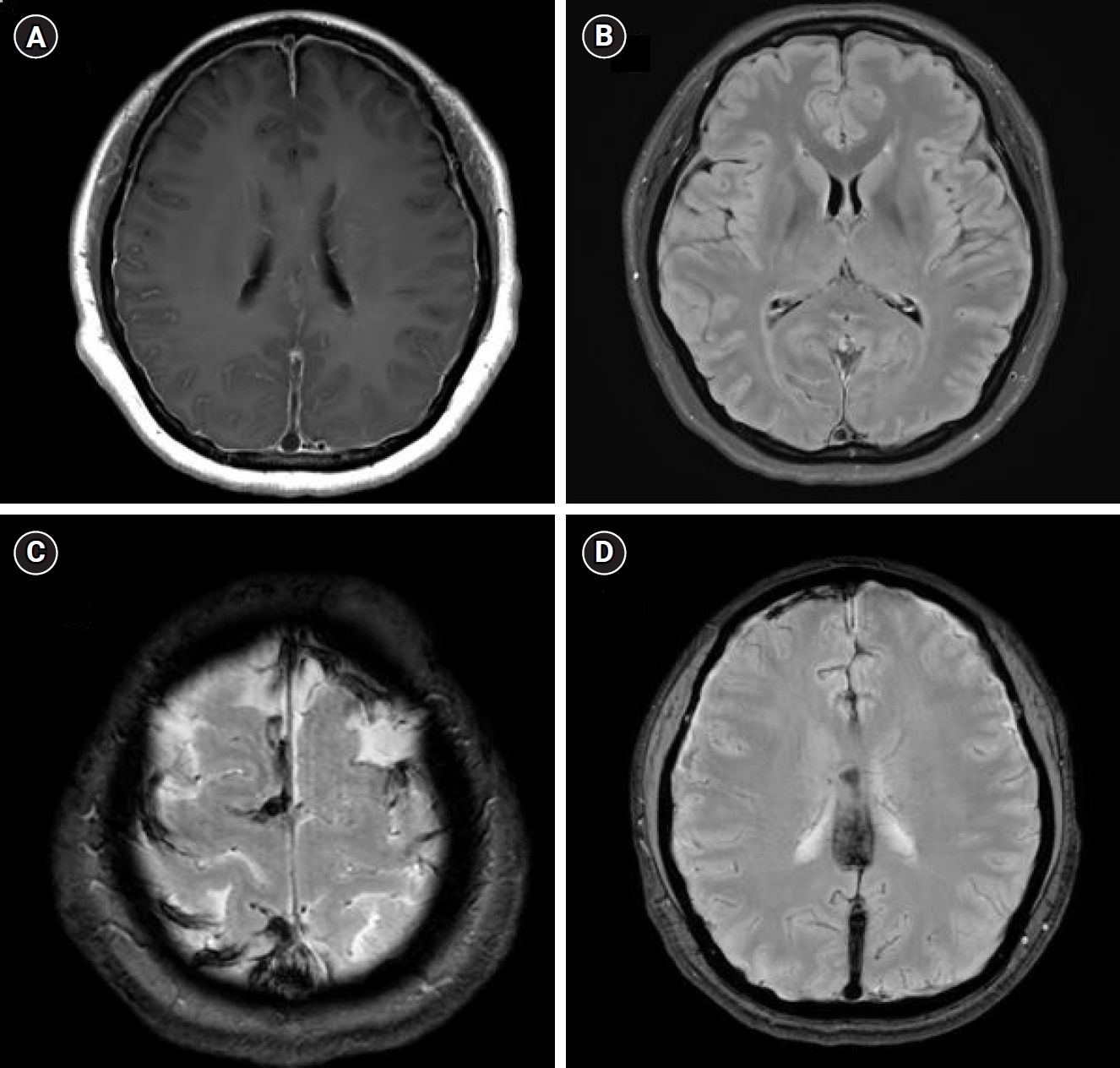
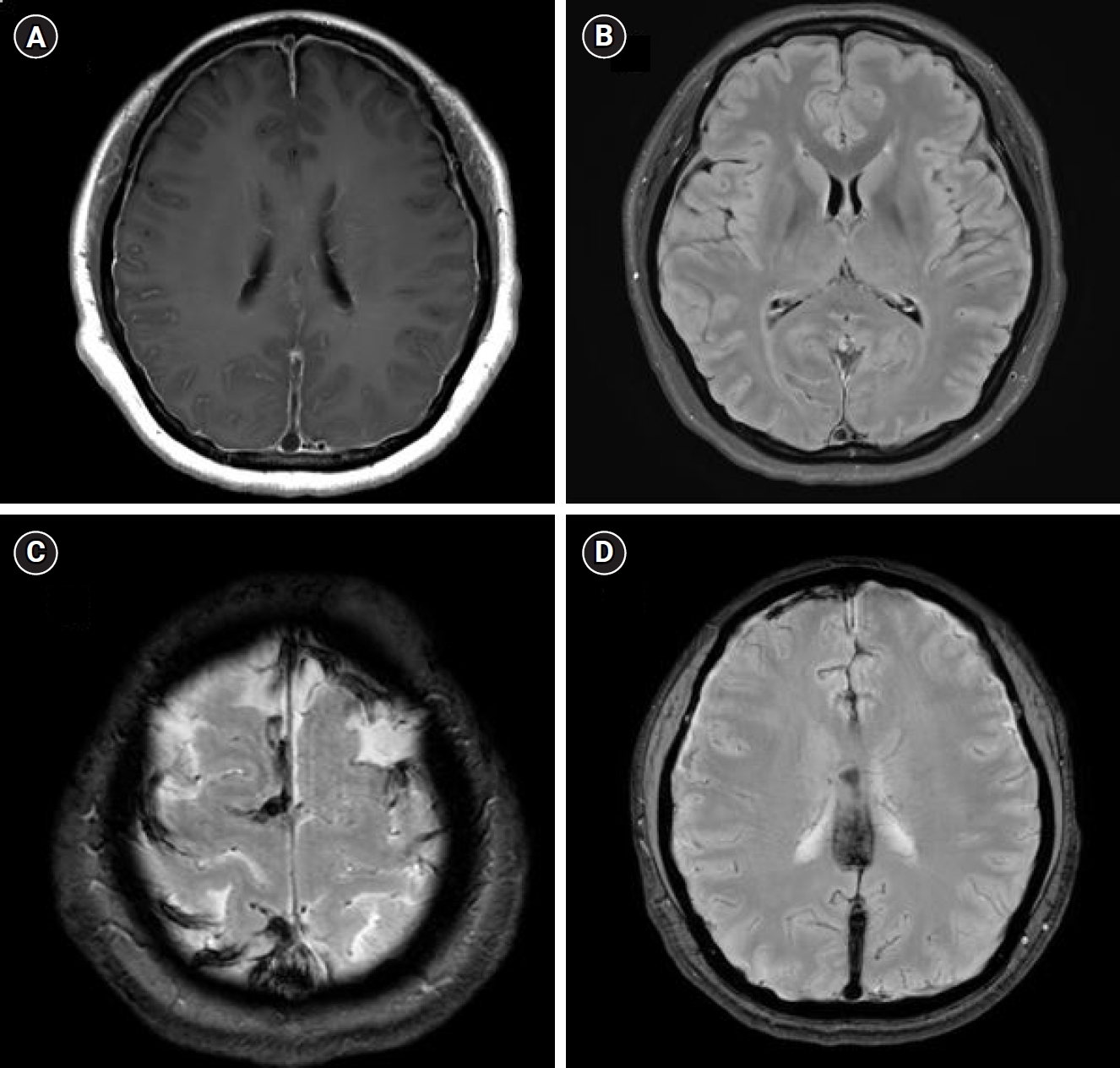
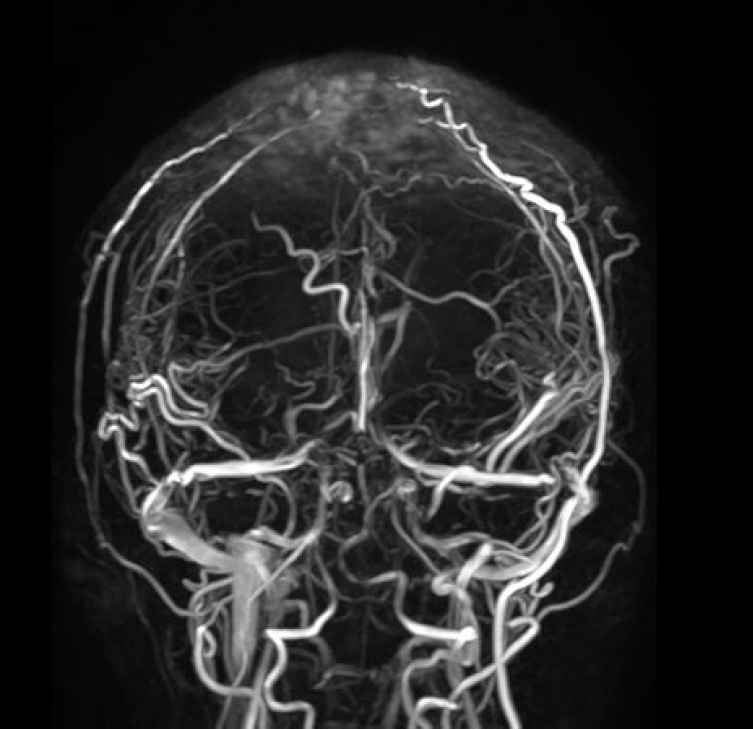
Magnetic resonance imaging (MRI) revealed signs consistent with SIH, including diffuse pachymeningeal enhancement, engorged venous sinuses, and subdural effusion along both cerebral convexity (Figure 1A, B). MRI also showed diffuse CVT in the superior sagittal sinus, bilateral transverse sinuses, straight sinus, and high frontoparietal cortical veins (Figure 1C, D). No definite diffusion-restricted lesion was observed.
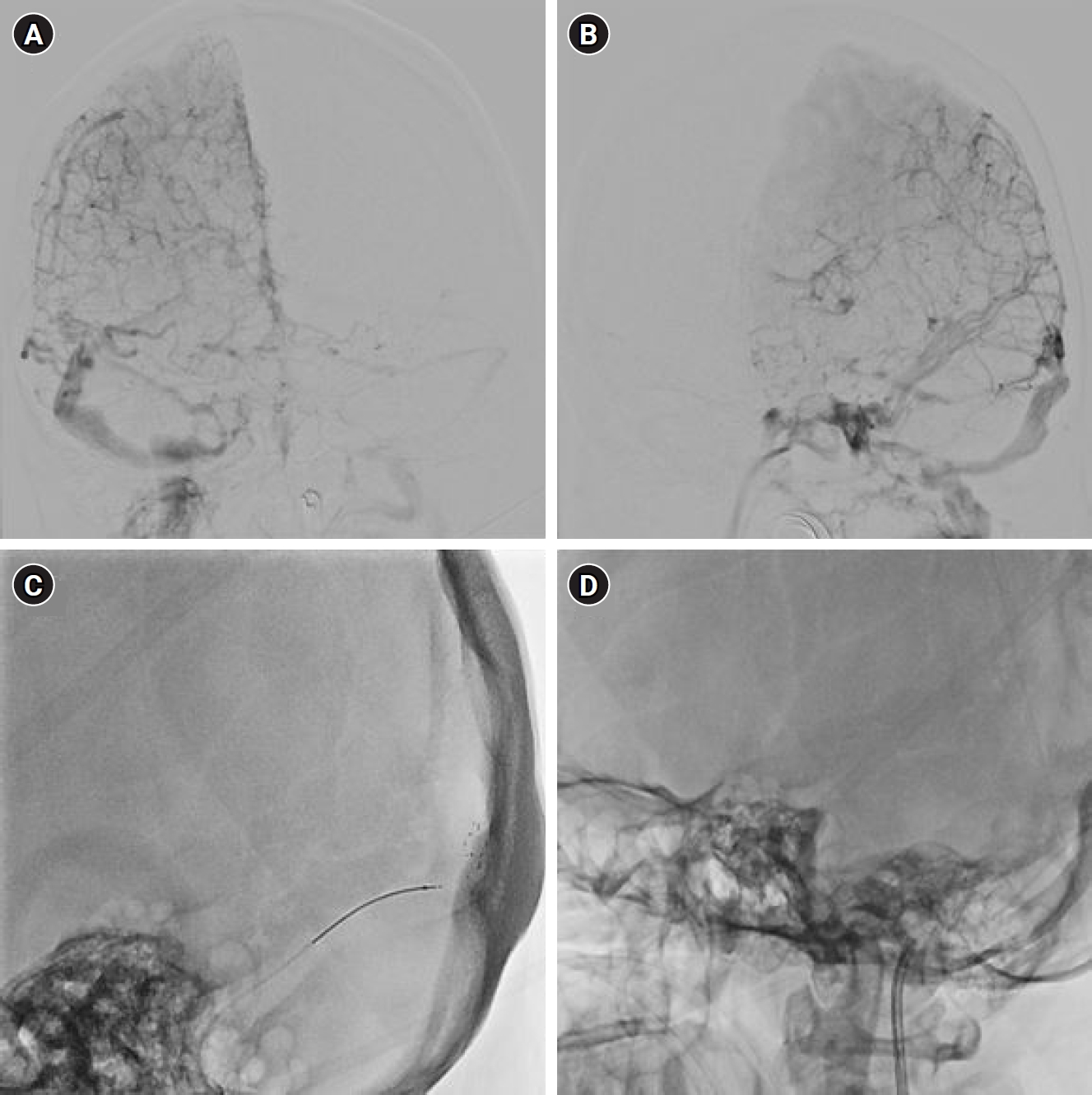
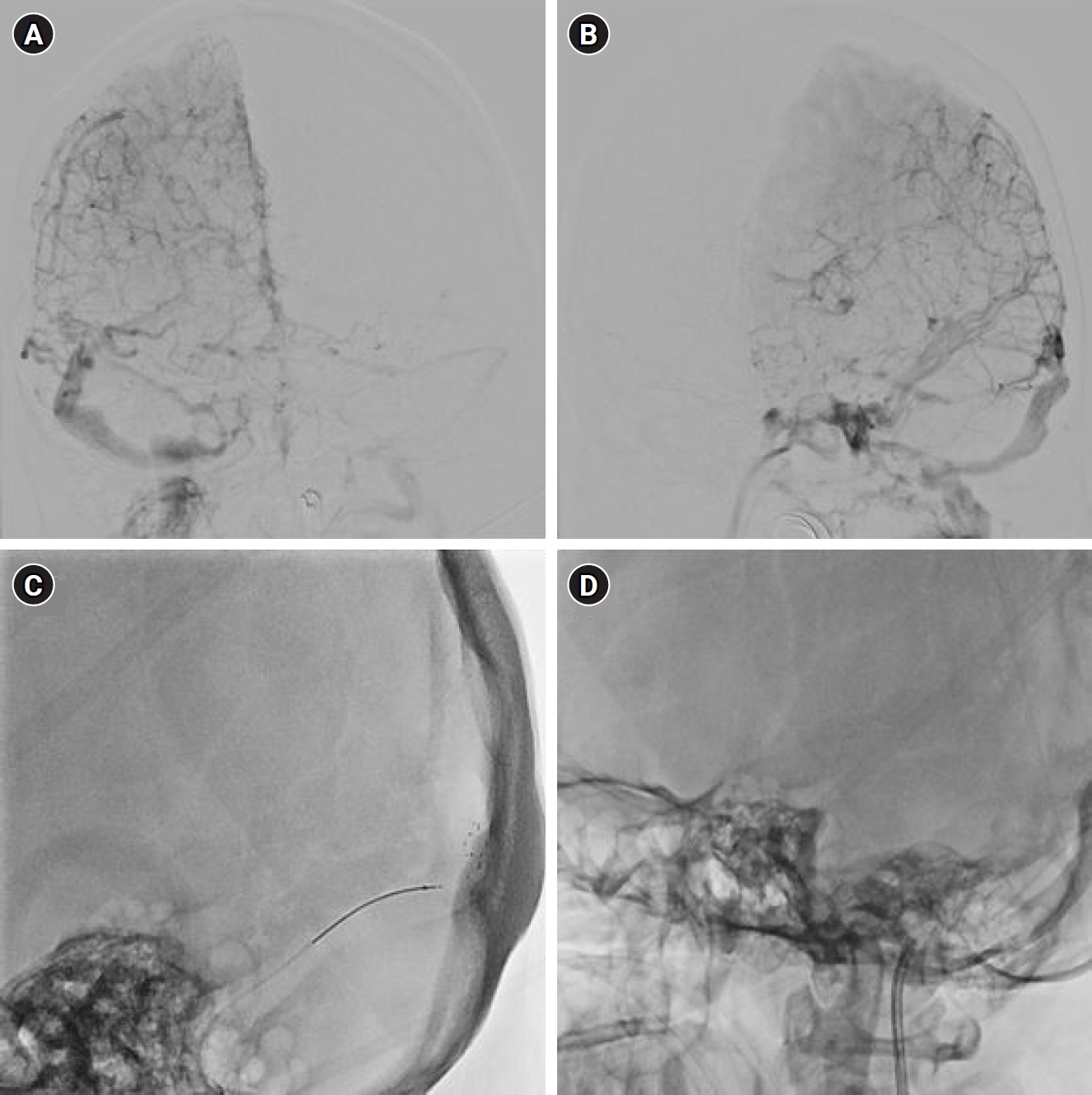
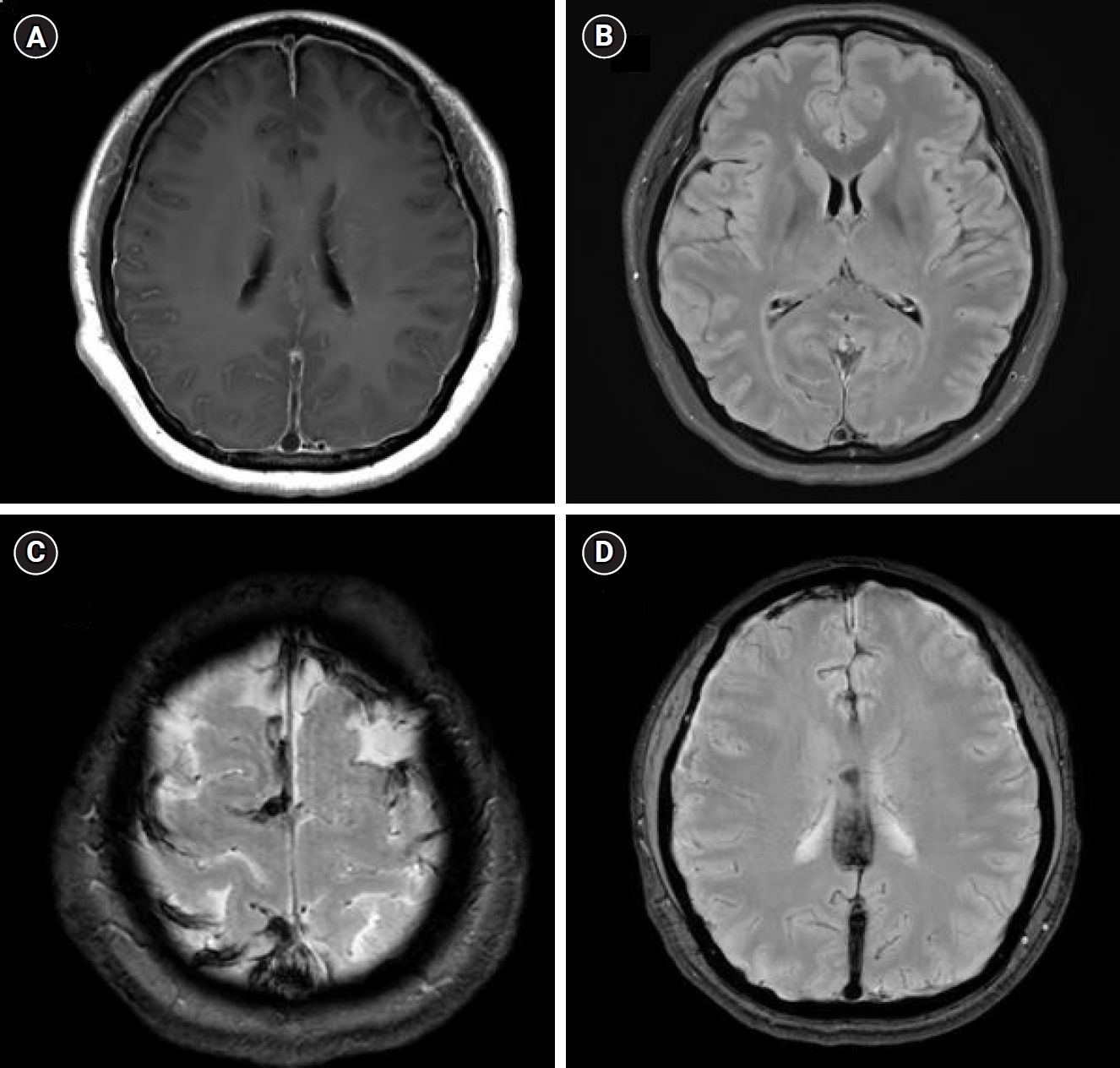
Given the severity of the CVT and the patient’s deteriorating neurological status, an endovascular approach was performed. Common carotid artery angiography confirmed occlusion of the venous sinuses, including the superior, inferior, straight, and bilateral transverse venous sinuses (Figure 2A, B). The solitaire X 6/40 mm retriever stent was deployed to cover the occluded segments and retrieved after 5 minutes. Subsequently, direct aspiration thrombectomy was performed using a reperfusion catheter (Figure 2C, D). Although a moderate amount of thrombus was removed and partial recanalization of straight sinus, vein of Galen, and bilateral transverse sinuses was achieved, occlusion of the superior sagittal sinus was still remained.
The patient showed significant neurological improvement in motor weakness within 48 hours post-thrombectomy, but the orthostatic headache persisted. Two days after thrombectomy, the patient underwent a lumbar puncture at the L3-4 level to confirm the opening pressure of 4 cm H2O, and blood patch using 20 mL of autologous blood at same level, which led to complete resolution of orthostatic headache.
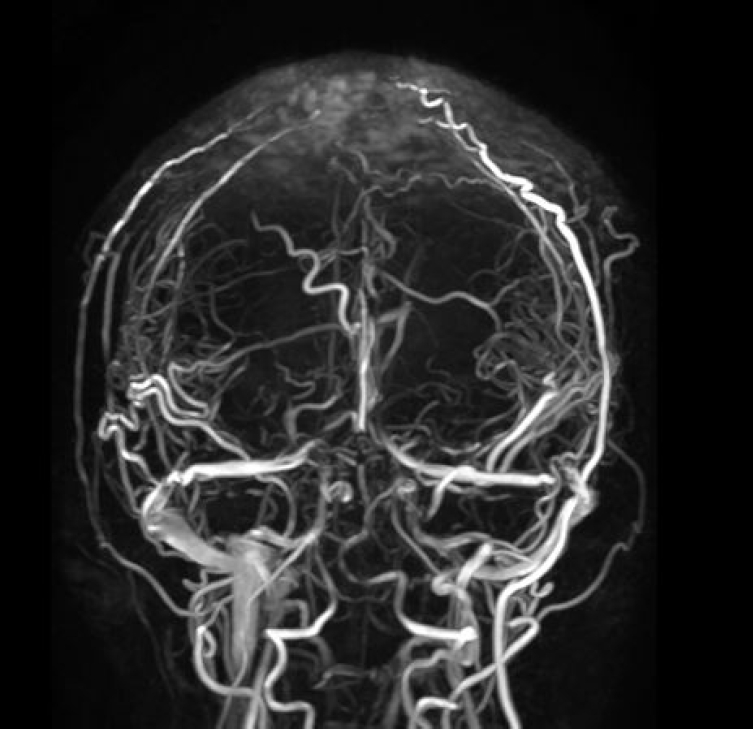
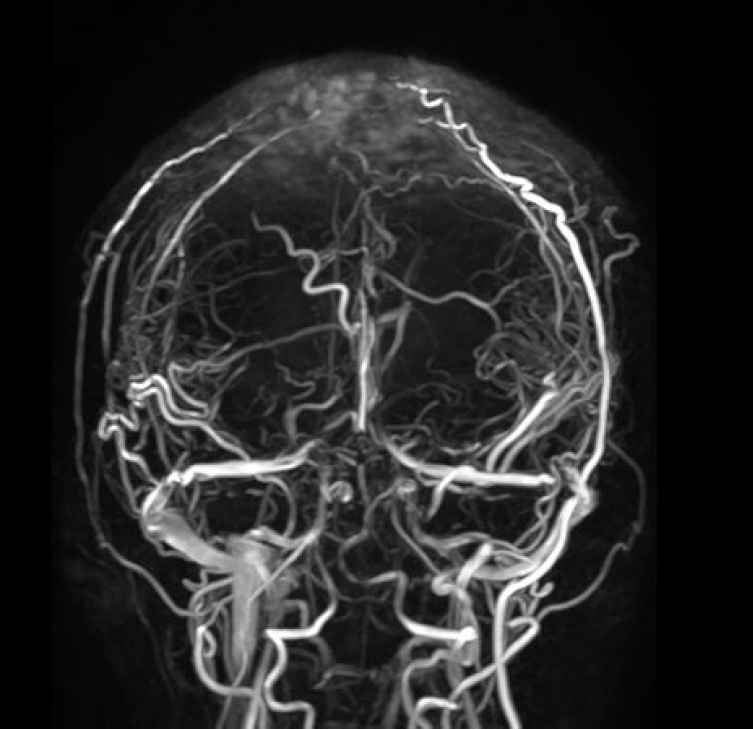
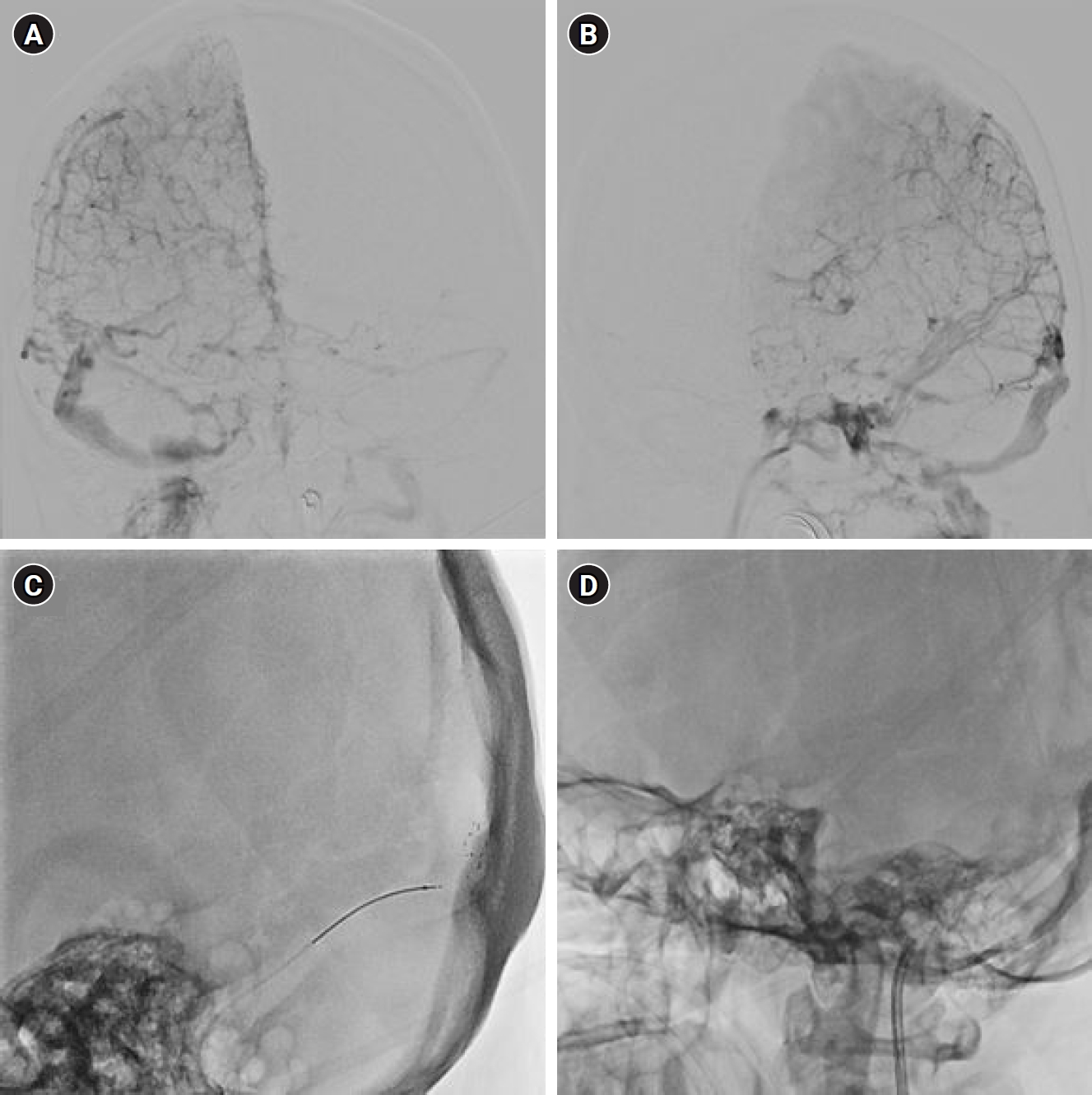
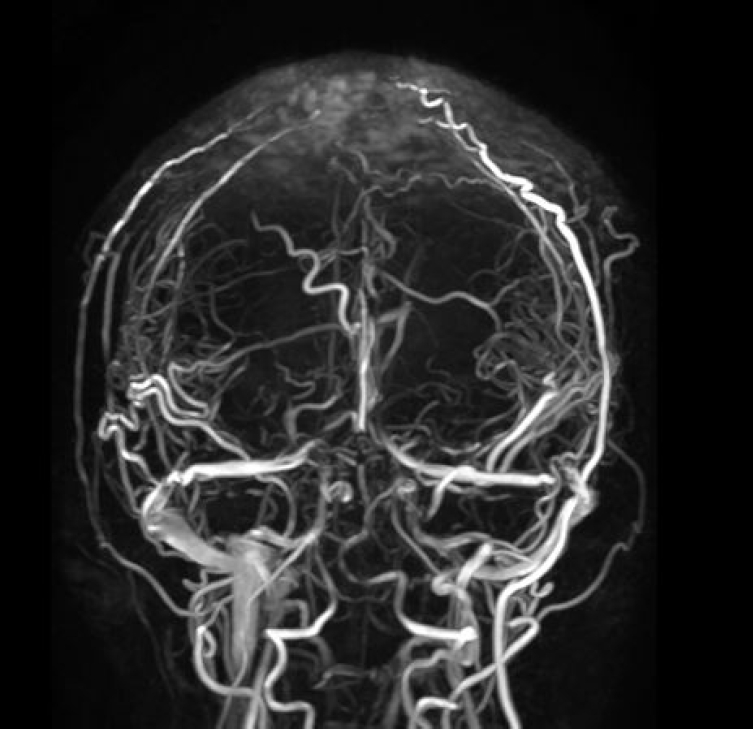
Follow-up magnetic resonance venography revealed residual CVT, and low-molecular-weight heparin anticoagulation therapy was continued (Figure 3). Upon discharge, the anticoagulation therapy was switched to a novel oral anticoagulant medication (apixaban 5 mg twice daily). There were no additional symptoms in the patient for 6 months after discharge, leading to discontinuation of anticoagulant therapy.
Thorough clinical examination and medical history revealed no other definitive cause for CVT in this patient, such as previous medical history, trauma, malignancy, or oral contraceptive use. Laboratory findings including complete blood count and coagulation panel, as well as C and S protein activities, were within normal limits. Additionally, autoimmune markers such as anti-neutrophil cytoplasmic antibody, rheumatoid factor, lupus anticoagulant, and antiphospholipid antibody tests, along with genetic testing for familial thrombophilia, all returned normal results. Therefore, based on the patient’s clinical history, disease progression, laboratory findings, and neuroimaging studies, the diagnosis of CVT secondary to SIH was established.
Retrieved thrombus from the patient was subjected to hematoxylin and eosin (H&E) staining, revealing a predominance of fibrin and platelets within the thrombus (thrombus composition: red blood cells [RBCs] 25%, fibrin/platelets 65%, and leukocytes 10%).
This case report was described in accordance with the CARE guidelines.
DISCUSSION
This case underscores the importance of considering CVT as a potential complication in patients with SIH and highlights the effectiveness of mechanical thrombectomy and epidural patch in managing CVT secondary to SIH. Additionally, this is the first histological analysis of retrieved thrombus from the CVT secondary to SIH. Although CVT secondary to SIH is considered rare, there have been numerous previous reports, indicating that it is not exceptionally uncommon. However, with novel pathological findings of fibrin/platelet predominant thrombus, this case sheds light on the pathological connection between CVT and SIH.
In this case, the patient initially presented with an orthostatic headache but later experienced a change in headache pattern to a thunderclap headache that persisted regardless of posture. Similarly, there have been previous studies where patients with SIH show changes in headache patterns and are subsequently found to have thrombosis.9-13 Existing studies on the temporal relationship between CVT and SIH highlight that SIH often precedes CVT.6,9 A causal link has not been established, but several hypotheses suggest mechanisms that could support the development of CVT following the onset of SIH. These include reduced venous blood flow due to venous engorgement, increased viscosity of cerebral venous content from diminished CSF reabsorption in the dural sinus, and mechanical distortion of the cerebral venous system.8
The thrombus extracted from the primary site of CVT caused by SIH can be used to evaluate the validity of the above-mentioned hypothesis. H&E staining is widely recognized as the gold standard in histology. In recent studies, H&E stain has been used to examine clot composition, categorizing clots from acute ischemic stroke, pulmonary embolism or deep vein thrombosis into groups such as RBC-rich, fibrin-rich, and mixed.14-18
The effects of thrombosis induced by reduced blood flow velocity, represented by platelet/fibrin dominance, surpass those of viscosity, represented by RBCs in the composition. In light of this, the identification of a fibrin/platelet dominant thrombus in this study can provide supporting evidence for CVT induced by SIH under conditions of low blood flow due to venous engorgement.19,20 Although there have been no reports on treatment or prognosis based on thrombus composition in CVT, there are reports indicating high mortality despite successful recanalization in ischemic stroke cases.21 Thrombectomy in severe CVT showed a reduction in complications and improvement in prognosis compared to medical treatment.22 Since the composition of the thrombus in CVT due to SIH suggests that possibility of high successful recanalization, thrombectomy may be considered as one of the treatment options.
Treatment for CVT complicated by SIH has not yet been established. In a literature review compiling case reports of CVT complicated by SIH, approximately half of the patients were found to have received anticoagulation therapy alone.6,9 Cases treated solely with epidural blood patch accounted for 20.0%, while those receiving anticoagulation and epidural blood patch treatments amounted to 22.8%.9 In our case, the patient represents the first documented case demonstrating successful outcomes following thrombectomy, epidural patch, and anticoagulation therapy. This case is significant as it demonstrates the improvement of CVT-induced weakness, without stroke, through thrombectomy; followed by the management of residual positional changes with epidural patch; and subsequent anticoagulation therapy for persistent CVT. The patient showed overall improvement without symptom recurrence, highlighting a favorable outcome.
This case has limitations, such as solely conducting H&E staining of thrombus. However, it holds value as a study demonstrating the safe implementation of various treatment methods and the confirmation of thrombus characteristics through them.
AVAILABILITY OF DATA AND MATERIAL
The data presented in this study are available upon reasonable request from the corresponding author.
AUTHOR CONTRIBUTIONS
Conceptualization: MKK, EYK; Data curation: MKK, HRS; Writing–original draft: MKK, EYK; Writing–review & editing: MKK, EYK, HRS.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING STATEMENT
Not applicable.
ACKNOWLEDGMENTS
We would like to express our gratitude to the Korean Headache Society for their invaluable support throughout the research.
Figure 1.Brain magnetic resonance imaging. (A) T1-gadolinium-enhanced axial view shows diffuse pachymeningeal enhancement. (B) A fluid-attenuated inversion recovery image indicates diffuse subdural effusion in both cerebral convexities. Gradient-echo imaging reveals a blooming effect along both the cortical veins (C) and the straight sagittal sinus (D).
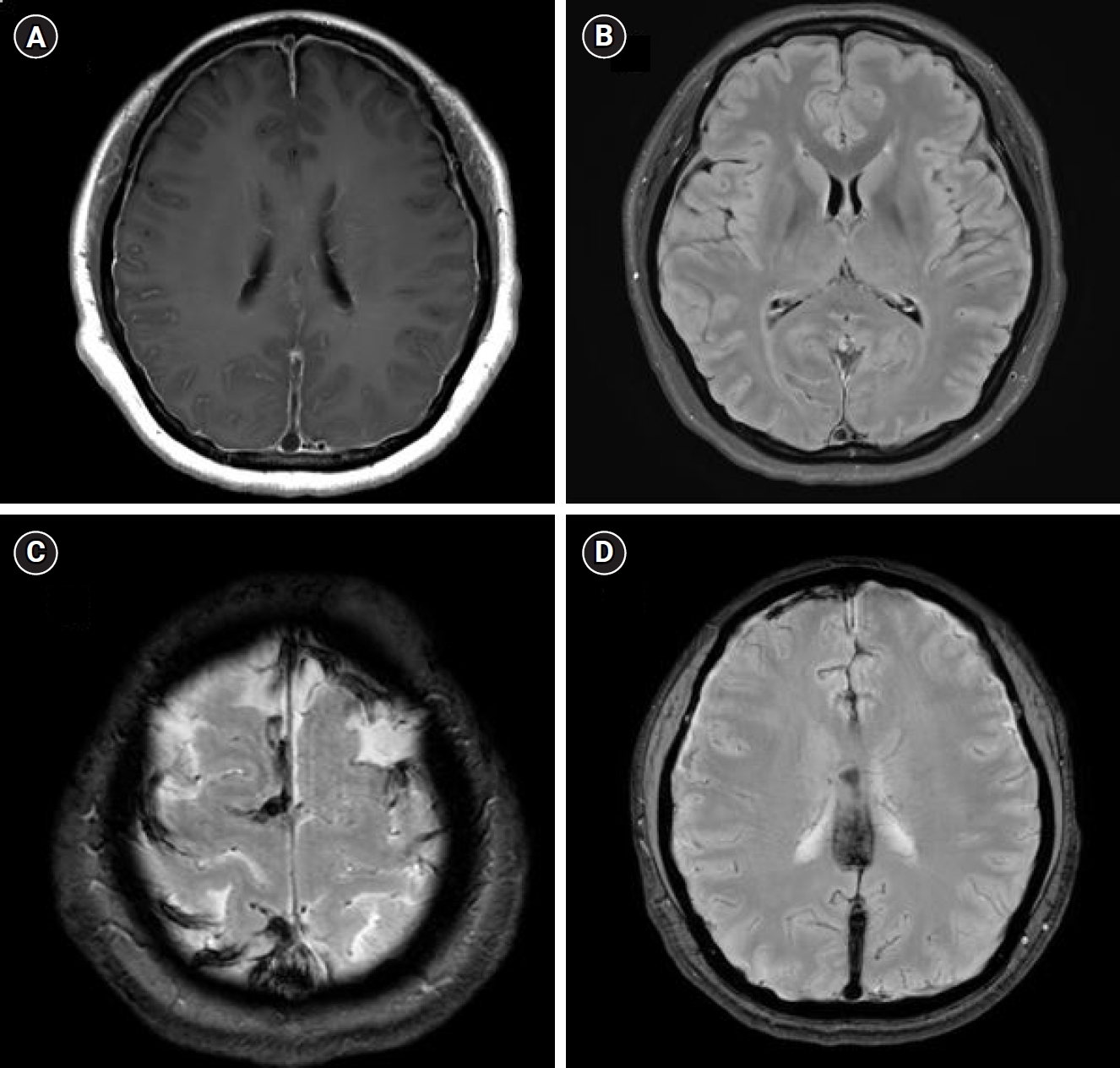
Figure 2.Venous phase of internal carotid artery angiography. (A, B) Angiography revealed occlusion in the superior, inferior, straight, and bilateral transverse venous sinuses. Stent-assisted mechanical thrombectomy (C) and direct aspiration thrombectomy (D) were performed.
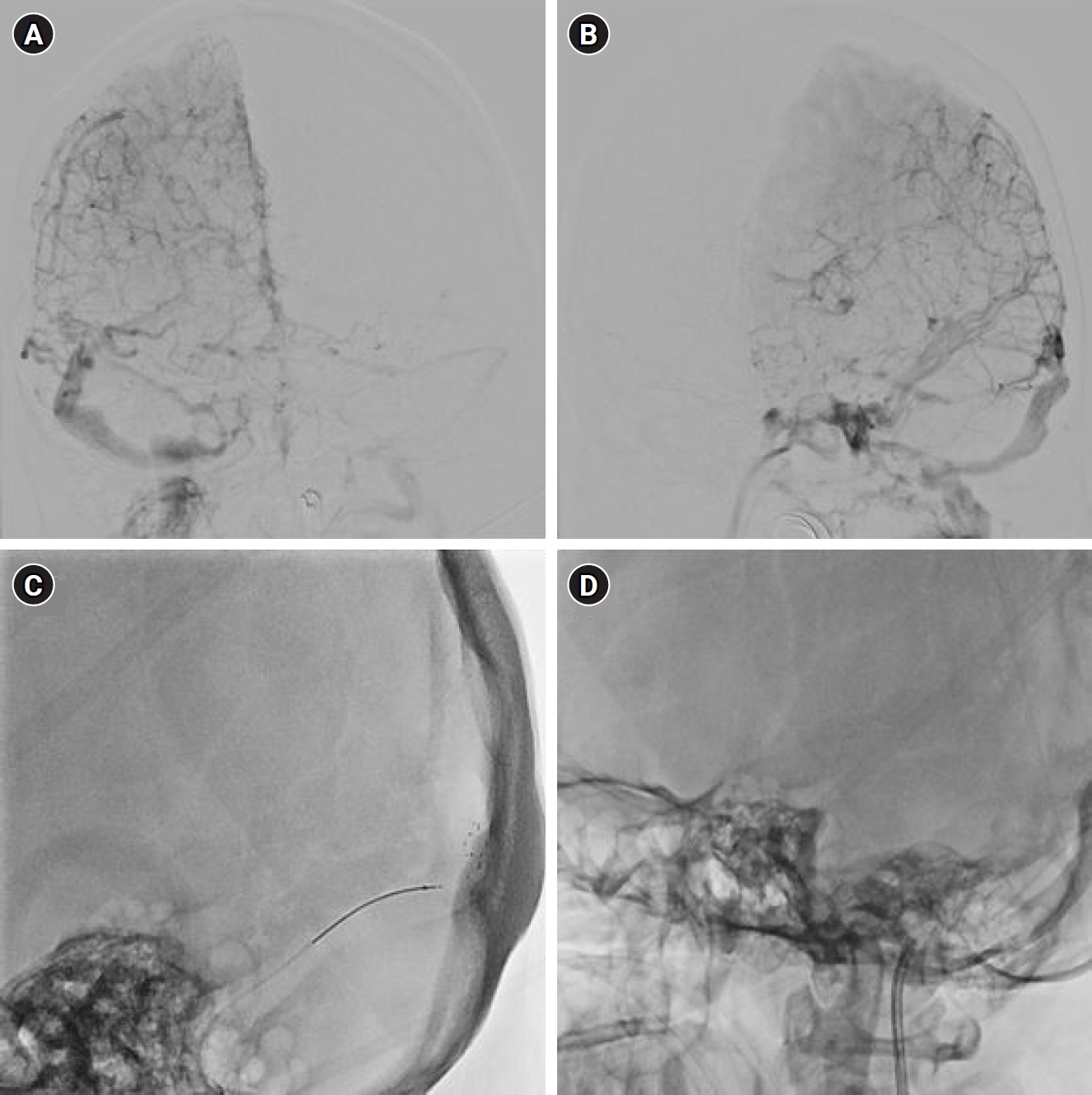
Figure 3.Brain magnetic resonance venography (MRV). MRV reveals occlusion of the superior sagittal sinus, with partial occlusion at the right transverse and sigmoid sinus junction.
REFERENCES
- 1. Marcelis J, Silberstein SD. Spontaneous low cerebrospinal fluid pressure headache. Headache 1990;30:192-196.ArticlePubMed
- 2. Silberstein SD, Marcelis J. Headache associated with changes in intracranial pressure. Headache 1992;32:84-94.ArticlePubMed
- 3. D’Antona L, Jaime Merchan MA, Vassiliou A, et al. Clinical presentation, investigation findings, and treatment outcomes of spontaneous intracranial hypotension syndrome: a systematic review and meta-analysis. JAMA Neurol 2021;78:329-337.ArticlePubMedPMC
- 4. Lai TH, Fuh JL, Lirng JF, Tsai PH, Wang SJ. Subdural haematoma in patients with spontaneous intracranial hypotension. Cephalalgia 2007;27:133-138.ArticlePubMedPDF
- 5. Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA 2006;295:2286-2296.ArticlePubMed
- 6. Schievink WI, Maya MM. Cerebral venous thrombosis in spontaneous intracranial hypotension. Headache 2008;48:1511-1519.ArticlePubMed
- 7. Costa P, Del Zotto E, Giossi A, et al. Headache due to spontaneous intracranial hypotension and subsequent cerebral vein thrombosis. Headache 2012;52:1592-1596.ArticlePubMed
- 8. Zhang D, Wang J, Zhang Q, He F, Hu X. Cerebral venous thrombosis in spontaneous intracranial hypotension: a report on 4 cases and a review of the literature. Headache 2018;58:1244-1255.ArticlePubMedPDF
- 9. Ferrante E, Trimboli M, Petrecca G, Allegrini F. Cerebral venous thrombosis in spontaneous intracranial hypotension: a report of 8 cases and review of the literature. J Neurol Sci 2021;425:117467.ArticlePubMed
- 10. Savoiardo M, Armenise S, Spagnolo P, et al. Dural sinus thrombosis in spontaneous intracranial hypotension: hypotheses on possible mechanisms. J Neurol 2006;253:1197-1202.ArticlePubMedPDF
- 11. Yoon KW, Cho MK, Kim YJ, Lee SK. Sinus thrombosis in a patient with intracranial hypotension: a suggested hypothesis of venous stasis. a case report. Interv Neuroradiol 2011;17:248-251.ArticlePubMedPMCPDF
- 12. Mao YT, Dong Q, Fu JH. Delayed subdural hematoma and cerebral venous thrombosis in a patient with spontaneous intracranial hypotension. Neurol Sci 2011;32:981-983.ArticlePubMedPDF
- 13. Garcia-Carreira MC, Vergé DC, Branera J, et al. Cerebral venous thrombosis in two patients with spontaneous intracranial hypotension. Case Rep Neurol Med 2014;2014:528268.ArticlePubMedPMCPDF
- 14. Hendley SA, Dimov A, Bhargava A, et al. Assessment of histological characteristics, imaging markers, and rt-PA susceptibility of ex vivo venous thrombi. Sci Rep 2021;11:22805.ArticlePubMedPMCPDF
- 15. Silver MJ, Kawakami R, Jolly MA, et al. Histopathologic analysis of extracted thrombi from deep venous thrombosis and pulmonary embolism: mechanisms and timing. Catheter Cardiovasc Interv 2021;97:1422-1429.ArticlePubMedPDF
- 16. Patil S, Darcourt J, Messina P, Bozsak F, Cognard C, Doyle K. Characterising acute ischaemic stroke thrombi: insights from histology, imaging and emerging impedance-based technologies. Stroke Vasc Neurol 2022;7:353-363.ArticlePubMedPMC
- 17. Bhambri A, Adapa AR, Liu Y, et al. Thrombus histology as it relates to mechanical thrombectomy: a meta-analysis and systematic review. Neurosurgery 2021;89:1122-1131.ArticlePubMedPDF
- 18. Boeckh-Behrens T, Kleine JF, Zimmer C, et al. Thrombus histology suggests cardioembolic cause in cryptogenic stroke. Stroke 2016;47:1864-1871.ArticlePubMed
- 19. Pivkin IV, Richardson PD, Karniadakis G. Blood flow velocity effects and role of activation delay time on growth and form of platelet thrombi. Proc Natl Acad Sci U S A 2006;103:17164-17169.ArticlePubMedPMC
- 20. Gersh KC, Nagaswami C, Weisel JW. Fibrin network structure and clot mechanical properties are altered by incorporation of erythrocytes. Thromb Haemost 2009;102:1169-1175.ArticlePubMedPMC
- 21. Hernández-Fernández F, Ramos-Araque ME, Barbella-Aponte R, et al. Fibrin-platelet clots in acute ischemic stroke. Predictors and clinical significance in a mechanical thrombectomy series. Front Neurol 2021;12:631343.ArticlePubMedPMC
- 22. Nepal G, Kharel S, Bhagat R, et al. Safety and efficacy of endovascular thrombectomy in patients with severe cerebral venous thrombosis: a meta-analysis. J Cent Nerv Syst Dis 2022;14:11795735221131736.ArticlePubMedPMCPDF
Citations
Citations to this article as recorded by

 , Eun Young Kim2,*
, Eun Young Kim2,* , Hye-Rim Shin3,*
, Hye-Rim Shin3,*

 PubReader
PubReader ePub Link
ePub Link Cite this Article
Cite this Article
 KHS
KHS