Articles
- Page Path
- HOME > Headache Pain Res > Volume 26(1); 2025 > Article
-
Review Article
Morning Headaches: An In-depth Review of Causes, Associated Disorders, and Management Strategies -
Yooha Hong1,*
 , Mi-Kyoung Kang1,*
, Mi-Kyoung Kang1,* , Min Seung Kim1
, Min Seung Kim1 , Heejung Mo1
, Heejung Mo1 , Rebecca C. Cox2
, Rebecca C. Cox2 , Hee-Jin Im1
, Hee-Jin Im1
-
Headache and Pain Research 2025;26(1):66-79.
DOI: https://doi.org/10.62087/hpr.2024.0023
Published online: January 17, 2025
1Department of Neurology, Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Republic of Korea
2Department of Psychological and Brain Sciences, Washington University in St. Louis, St. Louis, MO, USA
- Correspondence: Hee-Jin Im, M.D., Ph.D. Department of Neurology, Dongtan Sacred Heart Hospital, Hallym University College of Medicine, 7 Keunjaebong-gil, Hwaseong 18450, Republic of Korea Tel: +82-31-8086-3185, Fax: +82-31-8086-2317, E-mail: coolere@naver.com
- *These authors contributed equally to this study as co-first authors.
© 2025 The Korean Headache Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 51,635 Views
- 153 Download
Abstract
- Morning headaches, which are defined by occurrence upon or shortly after waking up in the morning, range from mild discomfort to severe pain and significantly impact an individual’s quality of life. Although morning headaches are a prevalent and potentially debilitating condition, the criteria for defining these headaches vary. The lack of universally accepted diagnostic criteria complicates understanding their etiology, associated factors, and potential interventions. The causes of morning headaches are multifaceted, including primary headache disorders like migraines and cluster headaches, and secondary causes such as sleep disorders, hypertension, abnormal intracranial pressure, and brain parenchymal diseases. Psychological factors, including anxiety and depression, as well as substance use, further complicate the clinical presentation, often requiring a multidisciplinary approach for effective diagnosis and treatment. This review provides a comprehensive overview of morning headaches, examining their various aspects and possible treatment options, with the goal of enhancing clinicians’ understanding and management of this common yet often overlooked condition.
INTRODUCTION
HEADACHE DISORDERS IN MORNING HEADACHE
1) Migraine
2) Cluster headache
3) Tension-type headache
4) Hypnic headache
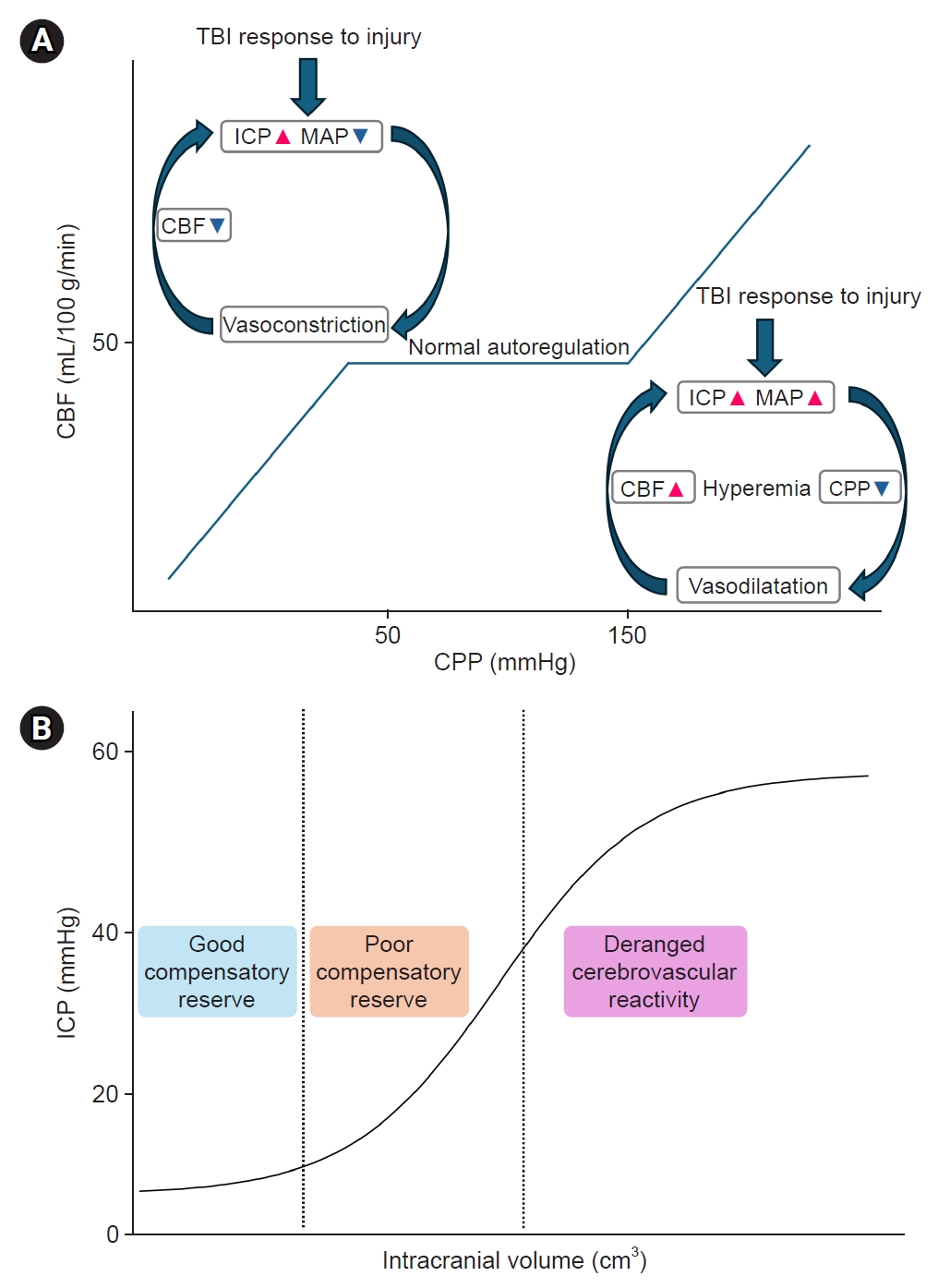
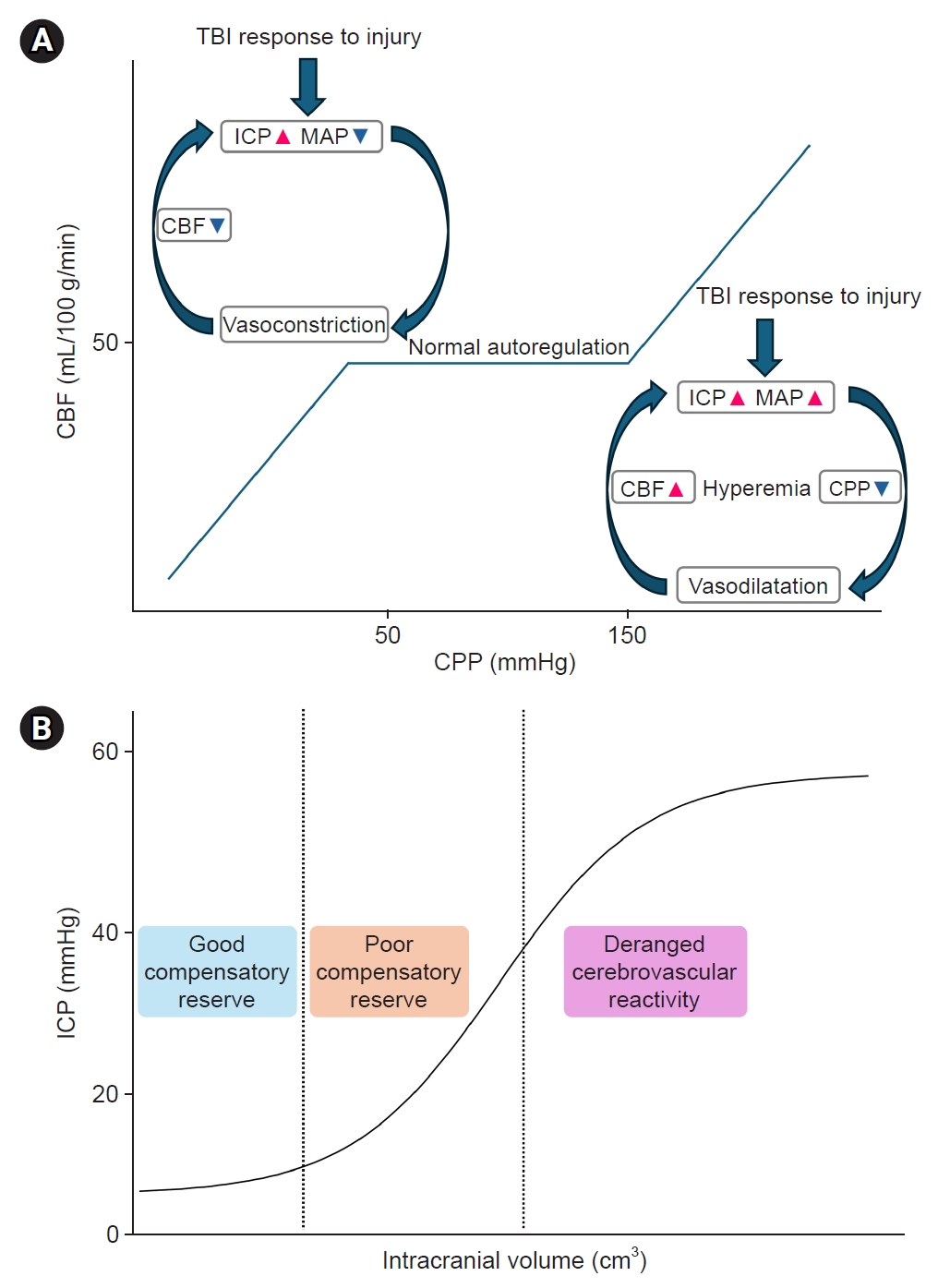
1) Intracranial pressure
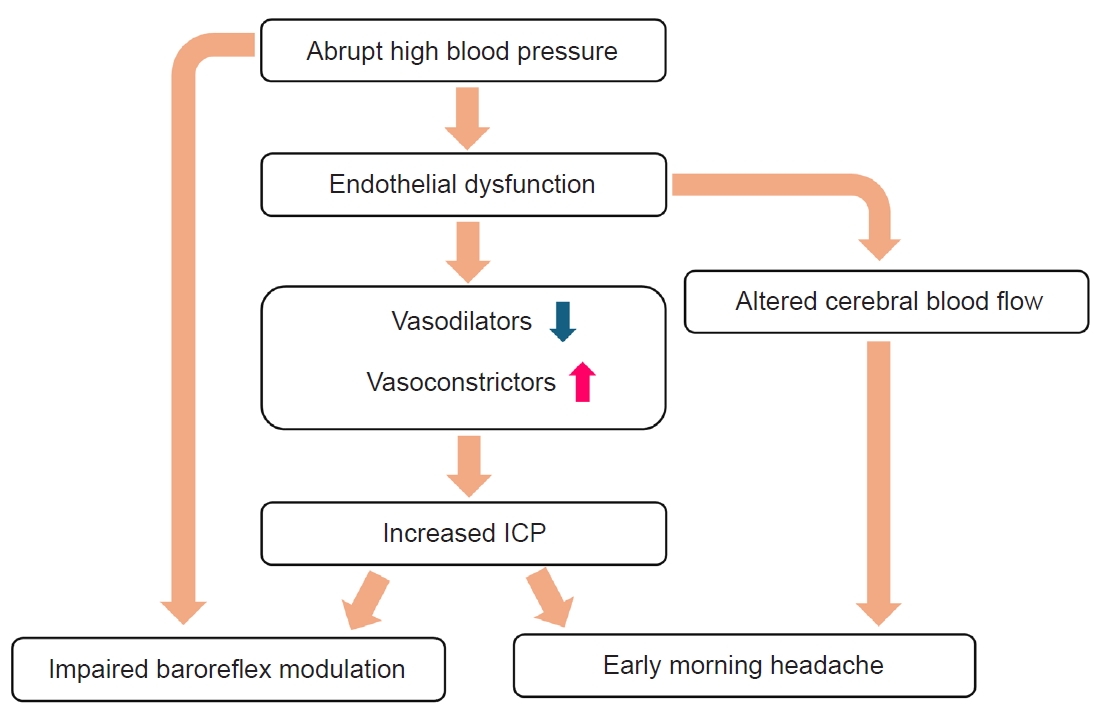
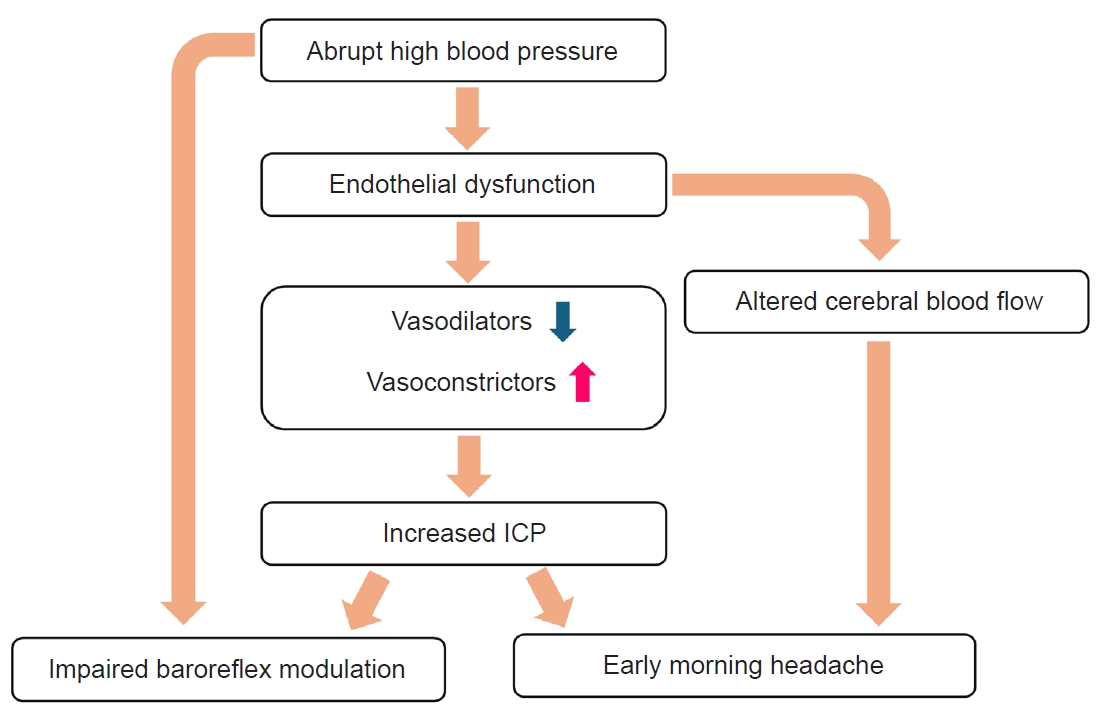
2) Hypertension and its complications
3) Brain tumor
SLEEP AND CIRCADIAN DISORDERS IN MORNING HEADACHE
BEHAVIORAL PROBLEMS IN MORNING HEADACHE
CONCLUSION
AVAILABILITY OF DATA AND MATERIAL
Not applicable.
AUTHOR CONTRIBUTIONS
Conceptualization: HJI; Data curation: YH, MKK, MSK, HM, RCC; Investigation: YH, MKK, MSK, HM, RCC; Writing–original draft: YH, MKK, MSK, HM, RCC; Writing–review and editing: YH, MKK, HJI.
CONFLICT OF INTEREST
Mi-Kyoung Kang has been the Editor of the Headache and Pain Research since September, 2023 and were not involved in the review process. The other authors has no other conflicts of interest to declare.
FUNDING STATEMENT
Not applicable.
ACKNOWLEDGMENTS
Not applicable.
Adapted from the article of Headache Classification Committee of the International Headache Society (Cephalalgia 2018;38:1-211).44
- 1. Ohayon MM. Prevalence and risk factors of morning headaches in the general population. Arch Intern Med 2004;164:97-102.ArticlePubMed
- 2. Russell MB, Kristiansen HA, Kværner KJ. Headache in sleep apnea syndrome: epidemiology and pathophysiology. Cephalalgia 2014;34:752-755.ArticlePubMedPDF
- 3. Goksan B, Gunduz A, Karadeniz D, et al. Morning headache in sleep apnoea: clinical and polysomnographic evaluation and response to nasal continuous positive airway pressure. Cephalalgia 2009;29:635-641.ArticlePubMedPDF
- 4. Lucchesi LM, Speciali JG, Santos-Silva R, Taddei JA, Tufik S, Bittencourt LR. Nocturnal awakening with headache and its relationship with sleep disorders in a population-based sample of adult inhabitants of Sao Paulo City, Brazil. Cephalalgia 2010;30:1477-1485.ArticlePubMedPDF
- 5. Gupta VK. Systemic hypertension, headache, and ocular hemodynamics: a new hypothesis. MedGenMed 2006;8:63.
- 6. Chen PK, Fuh JL, Lane HY, Chiu PY, Tien HC, Wang SJ. Morning headache in habitual snorers: frequency, characteristics, predictors and impacts. Cephalalgia 2011;31:829-836.ArticlePubMedPDF
- 7. Vgontzas A, Pavlović JM. Sleep disorders and migraine: review of literature and potential pathophysiology mechanisms. Headache 2018;58:1030-1039.ArticlePubMedPMCPDF
- 8. Kelman L, Rains JC. Headache and sleep: examination of sleep patterns and complaints in a large clinical sample of migraineurs. Headache 2005;45:904-910.ArticlePubMed
- 9. Lin YK, Lin GY, Lee JT, et al. Associations between sleep quality and migraine frequency: a cross-sectional case-control study. Medicine (Baltimore) 2016;95:e3554.ArticlePubMedPMC
- 10. Mishra S. What triggers morning migraines? Scientists might now know [Internet]. National Geographic; 2024 [cited 2024 Aug 3]. Available from: https://www.nationalgeographic.com/premium/article/migraine-prediction-mood-energy-sleep-stress
- 11. Seo JG. Menstrual migraine: a review of current research and clinical challenges. Headache Pain Res 2024;25:16-23.ArticlePDF
- 12. Kim SK. Migraine in women: inescapable femaleness? Headache Pain Res 2024;25:1-2.ArticlePDF
- 13. Kim S, Park JW. Migraines in women: a focus on reproductive events and hormonal milestones. Headache Pain Res 2024;25:3-15.ArticlePDF
- 14. Circadian Rhythms Bring on Headache Blues, Study Finds [Internet]. Psychiatrist; 2023 [cited 2024 Aug 3]. Available from: https://www.psychiatrist.com/news/circadian-rhythms-bring-on-headache-blues-study-finds/
- 15. Headaches and hormones: what’s the connection? [Internet]. Mayo Clinic; 2023 [cited 2024 Aug 3]. Available from: https://www.mayoclinic.org/diseases-conditions/chronic-daily-headaches/in-depth/headaches/art-20046729
- 16. Li K, Sun S, Xue Z, et al. Pre-attack and pre-episode symptoms in cluster headache: a multicenter cross-sectional study of 327 Chinese patients. J Headache Pain 2022;23:92.ArticlePubMedPMCPDF
- 17. Vieira KRM, Folchini CM, Heyde MDVD, Stuginski-Barbosa J, Kowacs PA, Piovesan EJ. Wake-up headache is associated with sleep bruxism. Headache 2020;60:974-980.ArticlePubMedPDF
- 18. Wei DY, Khalil M, Goadsby PJ. Managing cluster headache. Pract Neurol 2019;19:521-528.ArticlePubMedPMC
- 19. Hong Y, Kang MK, Chu MK, Cho SJ, Im HJ. Cluster headache characteristics and the severity of obstructive sleep apnea: insights from polysomnography analysis. Headache Pain Res 2024;25:63-71.ArticlePDF
- 20. Barloese M. Current understanding of the chronobiology of cluster headache and the role of sleep in its management. Nat Sci Sleep 2021;13:153-162.ArticlePubMedPMCPDF
- 21. Barloese M, Lund N, Petersen A, Rasmussen M, Jennum P, Jensen R. Sleep and chronobiology in cluster headache. Cephalalgia 2015;35:969-978.ArticlePubMedPDF
- 22. Pilati L, Torrente A, Alonge P, et al. Sleep and chronobiology as a key to understand cluster headache. Neurol Int 2023;15:497-507.ArticlePubMedPMC
- 23. Lund NLT, Petersen AS, Fronczek R, et al. Current treatment options for cluster headache: limitations and the unmet need for better and specific treatments-a consensus article. J Headache Pain 2023;24:121.ArticlePubMedPMCPDF
- 24. Barloese MC. Neurobiology and sleep disorders in cluster headache. J Headache Pain 2015;16:78.ArticlePubMedPMCPDF
- 25. Pergolizzi JV Jr, Magnusson P, LeQuang JA, Wollmuth C, Taylor R Jr, Breve F. Exploring the connection between sleep and cluster headache: a narrative review. Pain Ther 2020;9:359-371.ArticlePubMedPMCPDF
- 26. Nesbitt AD, Goadsby PJ. Cluster headache. BMJ 2012;344:e2407.ArticlePubMed
- 27. Kim M, Yu JK, Kim YH. Update on cluster headaches: from genetic to novel therapeutic approaches. Headache Pain Res 2024;25:42-53.ArticlePDF
- 28. Im HJ, Baek SH, Yun CH, Chu MK. Time preference of headache attack and chronotype in migraine and tension-type headache. Chronobiol Int 2019;36:1528-1536.ArticlePubMed
- 29. Tariq N, Estemalik E, Vij B, Kriegler JS, Tepper SJ, Stillman MJ. Long-term outcomes and clinical characteristics of hypnic headache syndrome: 40 patients series from a tertiary referral center. Headache 2016;56:717-724.ArticlePubMed
- 30. DeMaagd G. An introduction to hypnic headache. US Pharm 2021;46:17-20.
- 31. Lisotto C, Rossi P, Tassorelli C, Ferrante E, Nappi G. Focus on therapy of hypnic headache. J Headache Pain 2010;11:349-354.ArticlePubMedPMCPDF
- 32. Holle D, Naegel S, Obermann M. Pathophysiology of hypnic headache. Cephalalgia 2014;34:806-812.ArticlePubMedPDF
- 33. Holle D, Obermann M. Hypnic headache and caffeine. Expert Rev Neurother 2012;12:1125-1132.ArticlePubMed
- 34. Dolezil D, Mavrokordatos C. Hypnic headache: a rare primary headache disorder with very good response to indomethacin. Neuro Endocrinol Lett 2012;33:597-599.PubMed
- 35. Holle D, Naegel S, Krebs S, et al. Clinical characteristics and therapeutic options in hypnic headache. Cephalalgia 2010;30:1435-1442.ArticlePubMedPDF
- 36. Silberstein SD. Control of topiramate-induced paresthesias with supplemental potassium. Headache 2002;42:85.Article
- 37. Autunno M, Messina C, Blandino A, Rodolico C. Hypnic headache responsive to low-dose topiramate: a case report. Headache 2008;48:292-294.ArticlePubMed
- 38. Sibon I, Ghorayeb I, Henry P. Successful treatment of hypnic headache syndrome with acetazolamide. Neurology 2003;61:1157-1158.ArticlePubMed
- 39. Relja G, Zorzon M, Locatelli L, Carraro N, Antonello RM, Cazzato G. Hypnic headache: rapid and long-lasting response to prednisone in two new cases. Cephalalgia 2002;22:157-159.ArticlePubMedPDF
- 40. Rehmann R, Tegenthoff M, Zimmer C, Stude P. Case report of an alleviation of pain symptoms in hypnic headache via greater occipital nerve block. Cephalalgia 2017;37:998-1000.ArticlePubMedPDF
- 41. Friedman DI. Headaches due to low and high intracranial pressure. Continuum (Minneap Minn) 2018;24:1066-1091.ArticlePubMed
- 42. Wall M. The headache profile of idiopathic intracranial hypertension. Cephalalgia 1990;10:331-335.ArticlePubMedPDF
- 43. Ducros A, Biousse V. Headache arising from idiopathic changes in CSF pressure. Lancet Neurol 2015;14:655-668.ArticlePubMed
- 44. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018;38:1-211.ArticlePDF
- 45. Dobrocky T, Grunder L, Breiding PS, et al. Assessing spinal cerebrospinal fluid leaks in spontaneous intracranial hypotension with a scoring system based on brain magnetic resonance imaging findings. JAMA Neurol 2019;76:580-587.ArticlePubMedPMC
- 46. Courand PY, Serraille M, Girerd N, et al. The paradoxical significance of headache in hypertension. Am J Hypertens 2016;29:1109-1116.ArticlePubMedPDF
- 47. Janeway TC. A clinical study of hypertensive cardiovascular disease. Arch Intern Med (Chic) 1913;12:755-798.Article
- 48. Spałka J, Kędzia K, Kuczyński W, et al. Morning headache as an obstructive sleep apnea-related symptom among sleep clinic patients: a cross-section analysis. Brain Sci 2020;10:57.ArticlePubMedPMC
- 49. Genta-Pereira DC, Furlan SF, Omote DQ, et al. Nondipping blood pressure patterns predict obstructive sleep apnea in patients undergoing ambulatory blood pressure monitoring. Hypertension 2018;72:979-985.ArticlePubMed
- 50. Kario K. Nocturnal hypertension: new technology and evidence. Hypertension 2018;71:997-1009.ArticlePubMed
- 51. Finocchi C, Sassos D. Headache and arterial hypertension. Neurol Sci 2017;38:67-72.ArticlePDF
- 52. Hagen K, Stovner LJ, Vatten L, Holmen J, Zwart JA, Bovim G. Blood pressure and risk of headache: a prospective study of 22 685 adults in Norway. J Neurol Neurosurg Psychiatry 2002;72:463-466.ArticlePubMedPMC
- 53. Ruland S, Aiyagari V. Cerebral autoregulation and blood pressure lowering. Hypertension 2007;49:977-978.ArticlePubMed
- 54. Aaseth K, Grande RB, Kvaerner KJ, Gulbrandsen P, Lundqvist C, Russell MB. Prevalence of secondary chronic headaches in a population-based sample of 30-44-year-old persons. The Akershus study of chronic headache. Cephalalgia 2008;28:705-713.ArticlePubMedPDF
- 55. Pfund Z, Szapáry L, Jászberényi O, Nagy F, Czopf J. Headache in intracranial tumors. Cephalalgia 1999;19:787-765.ArticlePubMedPDF
- 56. Schankin CJ, Ferrari U, Reinisch VM, Birnbaum T, Goldbrunner R, Straube A. Characteristics of brain tumour-associated headache. Cephalalgia 2007;27:904-911.ArticlePubMedPDF
- 57. Forsyth PA, Posner JB. Headaches in patients with brain tumors: a study of 111 patients. Neurology 1993;43:1678-1683.ArticlePubMed
- 58. Valentinis L, Tuniz F, Valent F, et al. Headache attributed to intracranial tumours: a prospective cohort study. Cephalalgia 2010;30:389-398.ArticlePubMedPDF
- 59. Canac N, Jalaleddini K, Thorpe SG, Thibeault CM, Hamilton RB. Review: pathophysiology of intracranial hypertension and noninvasive intracranial pressure monitoring. Fluids Barriers CNS 2020;17:40.ArticlePubMedPMCPDF
- 60. Russo M, Villani V, Taga A, et al. Headache as a presenting symptom of glioma: a cross-sectional study. Cephalalgia 2018;38:730-735.ArticlePubMedPDF
- 61. Loghin M, Levin VA. Headache related to brain tumors. Curr Treat Options Neurol 2006;8:21-32.ArticlePubMedPDF
- 62. Palmieri A, Valentinis L, Zanchin G. Update on headache and brain tumors. Cephalalgia 2021;41:431-437.ArticlePubMedPDF
- 63. Boardman HF, Thomas E, Millson DS, Croft PR. Psychological, sleep, lifestyle, and comorbid associations with headache. Headache 2005;45:657-669.ArticlePubMedPDF
- 64. Rueda-Sánchez M, Díaz-Martínez LA. Prevalence and associated factors for episodic and chronic daily headache in the Colombian population. Cephalalgia 2008;28:216-225.ArticlePubMedPDF
- 65. Tran DP, Spierings EL. Headache and insomnia: their relation reviewed. Cranio 2013;31:165-170.ArticlePubMed
- 66. Spierings EL, Ranke AH, Honkoop PC. Precipitating and aggravating factors of migraine versus tension-type headache. Headache 2001;41:554-558.ArticlePubMed
- 67. Langemark M, Olesen J, Poulsen DL, Bech P. Clinical characterization of patients with chronic tension headache. Headache 1988;28:590-596.ArticlePubMed
- 68. Cho SJ, Chu MK. Risk factors of chronic daily headache or chronic migraine. Curr Pain Headache Rep 2015;19:465.ArticlePubMedPDF
- 69. Lund N, Westergaard ML, Barloese M, Glümer C, Jensen RH. Epidemiology of concurrent headache and sleep problems in Denmark. Cephalalgia 2014;34:833-845.ArticlePubMedPDF
- 70. Blau JN. Sleep deprivation headache. Cephalalgia 1990;10:157-160.ArticlePubMedPDF
- 71. Jennum P, Jensen R. Sleep and headache. Sleep Med Rev 2002;6:471-479.ArticlePubMed
- 72. Lateef TM, Dey D, Leroux A, et al. Association between electronic diary-rated sleep, mood, energy, and stress with incident headache in a community-based sample. Neurology 2024;102:e208102.ArticlePubMed
- 73. Ran C, Jennysdotter Olofsgård F, Steinberg A, et al. Patients with cluster headache show signs of insomnia and sleep related stress: results from an actigraphy and self-assessed sleep study. J Headache Pain 2023;24:114.ArticlePubMedPMCPDF
- 74. Malu OO, Bailey J, Hawks MK. Cluster headache: rapid evidence review. Am Fam Physician 2022;105:24-32.PubMed
- 75. Song TJ, Lee MJ, Choi YJ, et al. Differences in characteristics and comorbidity of cluster headache according to the presence of migraine. J Clin Neurol 2019;15:334-338.ArticlePubMedPMCPDF
- 76. Seo MY, Lee MK, Han MS, Yoo J, Lee SH. Improvement of morning headache in adults with obstructive sleep apnea after positive airway pressure therapy. Sci Rep 2023;13:14620.ArticlePubMedPMCPDF
- 77. Suzuki K, Miyamoto M, Miyamoto T, et al. Sleep apnoea headache in obstructive sleep apnoea syndrome patients presenting with morning headache: comparison of the ICHD-2 and ICHD-3 beta criteria. J Headache Pain 2015;16:56.ArticlePubMedPMCPDF
- 78. Rains JC, Poceta JS. Headache and sleep disorders: review and clinical implications for headache management. Headache 2006;46:1344-1363.ArticlePubMed
- 79. Stark CD, Stark RJ. Sleep and chronic daily headache. Curr Pain Headache Rep 2015;19:468.ArticlePubMedPDF
- 80. Lovati C. Sleep apnea headache and headaches with sleep apnea: the importance of being secondary. Expert Rev Neurother 2013;13:1135-1137.ArticlePubMed
- 81. Ulfberg J, Carter N, Talbäck M, Edling C. Headache, snoring and sleep apnoea. J Neurol 1996;243:621-625.ArticlePubMedPDF
- 82. Kristiansen HA, Kværner KJ, Akre H, Øverland B, Sandvik L, Russell MB. Sleep apnoea headache in the general population. Cephalalgia 2012;32:451-458.ArticlePubMedPDF
- 83. Aldrich MS, Chauncey JB. Are morning headaches part of obstructive sleep apnea syndrome? Arch Intern Med 1990;150:1265-1267.ArticlePubMed
- 84. Sand T, Hagen K, Schrader H. Sleep apnoea and chronic headache. Cephalalgia 2003;23:90-95.ArticlePubMedPDF
- 85. van Oosterhout W, van Someren E, Schoonman GG, et al. Chronotypes and circadian timing in migraine. Cephalalgia 2018;38:617-625.ArticlePubMedPDF
- 86. Pringsheim T. Cluster headache: evidence for a disorder of circadian rhythm and hypothalamic function. Can J Neurol Sci 2002;29:33-40.ArticlePubMed
- 87. Alstadhaug K, Salvesen R, Bekkelund S. 24-hour distribution of migraine attacks. Headache 2008;48:95-100.ArticlePubMed
- 88. Gori S, Morelli N, Maestri M, Fabbrini M, Bonanni E, Murri L. Sleep quality, chronotypes and preferential timing of attacks in migraine without aura. J Headache Pain 2005;6:258-260.ArticlePubMedPMCPDF
- 89. Jones BE. From waking to sleeping: neuronal and chemical substrates. Trends Pharmacol Sci 2005;26:578-586.ArticlePubMed
- 90. Jones BE. Arousal and sleep circuits. Neuropsychopharmacology 2020;45:6-20.ArticlePubMedPDF
- 91. de Tommaso M, Delussi M. Circadian rhythms of migraine attacks in episodic and chronic patients: a cross sectional study in a headache center population. BMC Neurol 2018;18:94.ArticlePubMedPMC
- 92. Poulsen AH, Younis S, Thuraiaiyah J, Ashina M. The chronobiology of migraine: a systematic review. J Headache Pain 2021;22:76.ArticlePubMedPMCPDF
- 93. Lake AE 3rd, Rains JC, Penzien DB, Lipchik GL. Headache and psychiatric comorbidity: historical context, clinical implications, and research relevance. Headache 2005;45:493-506.ArticlePubMedPDF
- 94. Breslau N, Merikangas K, Bowden CL. Comorbidity of migraine and major affective disorders. Neurology 1994;44:S17-S22.
- 95. Puca F, Genco S, Prudenzano MP, et al. Psychiatric comorbidity and psychosocial stress in patients with tension-type headache from headache centers in Italy. The Italian Collaborative Group for the Study of Psychopathological Factors in Primary Headaches. Cephalalgia 1999;19:159-164.ArticlePubMed
- 96. Verri AP, Proietti Cecchini A, Galli C, Granella F, Sandrini G, Nappi G. Psychiatric comorbidity in chronic daily headache. Cephalalgia 1998;18 Suppl 21:45-49.ArticlePubMed
- 97. Karsan N, Goadsby PJ. Migraine is more than just headache: is the link to chronic fatigue and mood disorders simply due to shared biological systems? Front Hum Neurosci 2021;15:646692.ArticlePubMedPMC
- 98. Seidel S, Frantal S, Oberhofer P, et al. Morning headaches in snorers and their bed partners: a prospective diary study. Cephalalgia 2012;32:888-895.ArticlePubMedPDF
- 99. Panconesi A. Alcohol and migraine: trigger factor, consumption, mechanisms. A review. J Headache Pain 2008;9:19-27.ArticlePubMedPMCPDF
- 100. Yokoyama M, Suzuki N, Yokoyama T, et al. Interactions between migraine and tension-type headache and alcohol drinking, alcohol flushing, and hangover in Japanese. J Headache Pain 2012;13:137-145.ArticlePubMedPMCPDF
- 101. Sjaastad O, Bakketeig LS. Caffeine-withdrawal headache. The Vågå study of headache epidemiology. Cephalalgia 2004;24:241-249.ArticlePubMedPDF
- 102. Mostofsky E, Mittleman MA, Buettner C, Li W, Bertisch SM. Prospective cohort study of caffeinated beverage intake as a potential trigger of headaches among migraineurs. Am J Med 2019;132:984-991.ArticlePubMedPMC
- 103. Silverman K, Evans SM, Strain EC, Griffiths RR. Withdrawal syndrome after the double-blind cessation of caffeine consumption. N Engl J Med 1992;327:1109-1114.ArticlePubMed
- 104. Striley CL, Griffiths RR, Cottler LB. Evaluating dependence criteria for caffeine. J Caffeine Res 2011;1:219-225.ArticlePubMedPMC
- 105. Evans SM, Griffiths RR. Caffeine withdrawal: a parametric analysis of caffeine dosing conditions. J Pharmacol Exp Ther 1999;289:285-294.ArticlePubMed
- 106. Phillips-Bute BG, Lane JD. Caffeine withdrawal symptoms following brief caffeine deprivation. Physiol Behav 1997;63:35-39.ArticlePubMed
- 107. Ashina S, Terwindt GM, Steiner TJ, et al. Medication overuse headache. Nat Rev Dis Primers 2023;9:5.ArticlePubMedPDF
- 108. Cheung V, Amoozegar F, Dilli E. Medication overuse headache. Curr Neurol Neurosci Rep 2015;15:509.ArticlePubMedPDF
REFERENCES
Figure & Data
References
Citations

 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
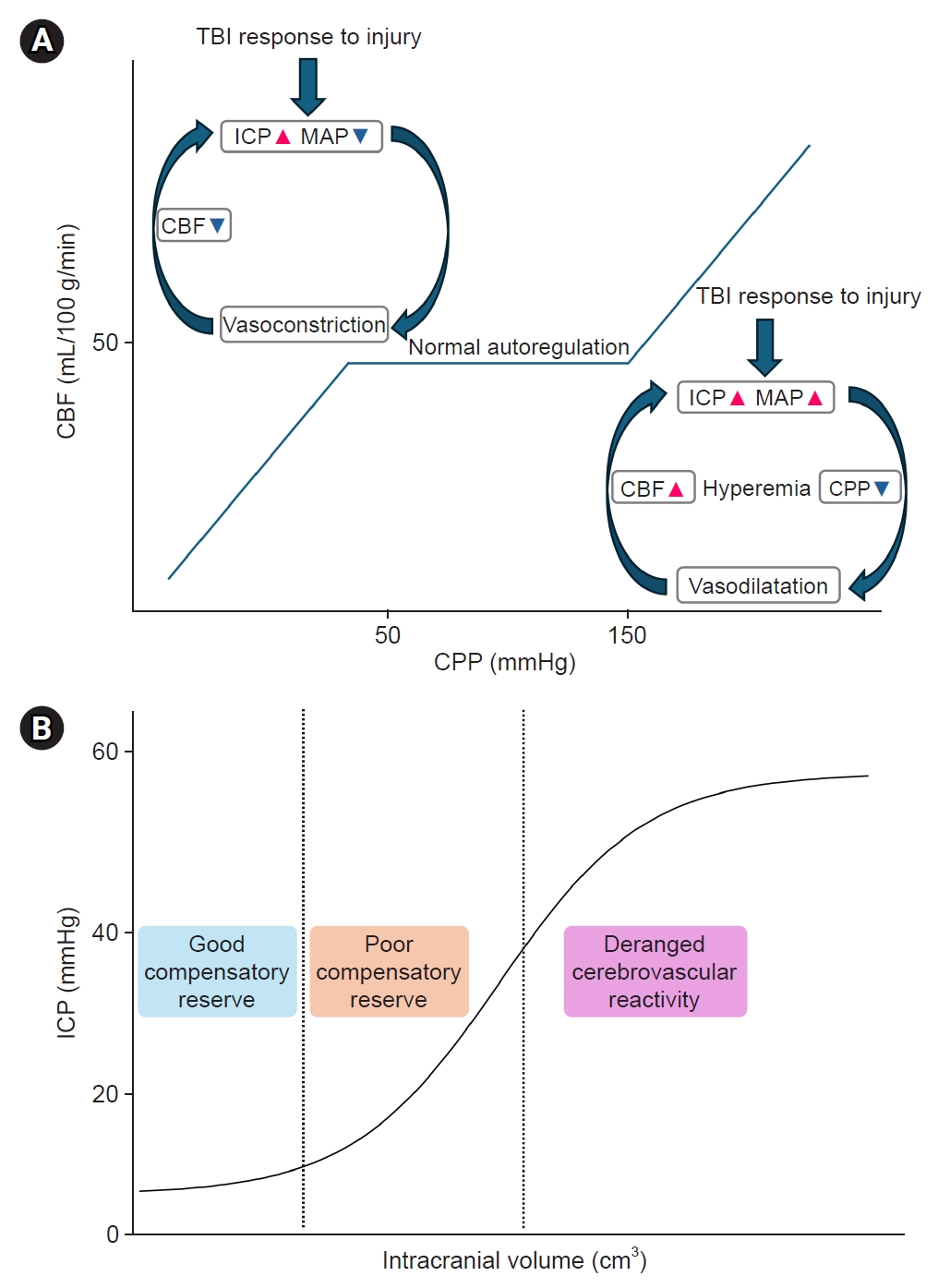
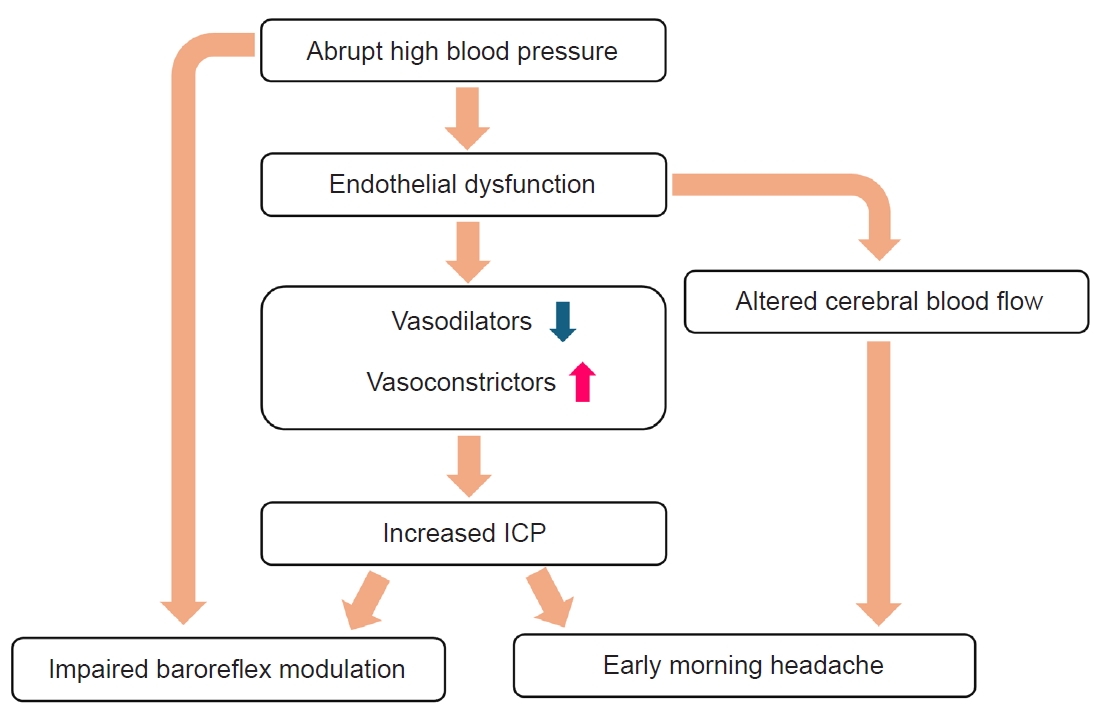
Figure 1.
Figure 2.
| 1. Headache has developed in temporal relation to the onset of sleep apnea |
| 2. Either or both of the following: |
| a) headache has worsened in parallel with worsening of sleep apnea |
| b) headache has significantly improved or remitted in parallel with improvement in or resolution of sleep apnea |
| 3. Headache has at least one of the following three characteristics: |
| a) recurring on ≥15 days/mo |
| b) all of the following: |
| – bilateral location |
| – pressing quality |
| – not accompanied by nausea, photophobia or phonophobia |
| c) resolving within 4 hours |
| 4. Not better accounted for by another ICHD-3 diagnosis. |
| Risk factors | Neurologist’s considerations | Treatment options |
|---|---|---|
| Primary headaches | -Distinguish between primary headache disorders (e.g., migraine, cluster headache, hypnic headache) that may present as morning headaches | -Pharmacological management: pain-relieving, preventive medications |
| -Rule out secondary causes of headaches | -Non-pharmacological management: behavioral therapy (regular sleep, exercise, avoidance of trigger factors, Biofeedback) | |
| Secondary headaches | -Distinguish between primary and secondary headache disorders | -Imaging studies (MRI/MRA, CT) |
| -Rule out brain parenchymal lesion or abnormal intracranial pressure | -Lumbar puncture if indicated | |
| -Monitor for red flag symptoms | -Medication to reduce intracranial pressure or antiplatelet therapy if indicated | |
| -Evaluate stroke risk | -Management of vascular risk factors | |
| -Monitor blood pressure regularly, lifestyle changes, medication as prescribed by a doctor | ||
| Sleep disorders | -Evaluate for secondary headaches & potential underlying neurological symptoms | -PAP for sleep apnea |
| -Take a sleep history in detailed/assess the sleep quality | -Sleep hygiene education for insomnia | |
| -Consider polysomnography for diagnosis | -Cognitive behavioral therapy for insomnia | |
| -Assess for mood disorders often comorbid with sleep issues | -Light therapy, chronotherapy | |
| -Melatonin or sleeping pills supplementation (*teeth grinding or sleep posture problems: use of a night guard, dental treatment, supportive pillows, physical therapy) | ||
| Cervicogenic factors | -Assess for cervical spine pathology | -Physical therapy |
| -Consider contribution to other headache types | -Occipital nerve blocks | |
| -Evaluate for comorbid temporomandibular disorders | -Postural correction | |
| Substance use (medication, caffeine/alcohol) | -Evaluate for medication-overuse headache | -Medication withdrawal under supervision |
| -Assess for substance use disorders | -Preventive medications | |
| -Consider comorbid psychiatric conditions | -Patient education on medication use | |
| -Develop personalized withdrawal plans | -Gradual caffeine reduction | |
| -Educate on caffeine’s role in headaches | -Alcohol moderation or abstinence | |
| -Hydration therapy | ||
| Psychiatric comorbidities | -Screen for psychiatric comorbidities | - Psychotherapy |
| -Consider impact on headache chronification | - Antidepressants with analgesic properties | |
| -Evaluate need for a multidisciplinary approach | - Stress management |
Adapted from the article of Headache Classification Committee of the International Headache Society (Cephalalgia 2018;38:1-211).
MRI, magnetic resonance imaging; MRA, magnetic resonance angiography; CT, computed tomography; PAP, positive airway pressure.
Table 1.
Table 2.
TOP
 KHS
KHS