Articles
- Page Path
- HOME > Headache Pain Res > Volume 26(2); 2025 > Article
-
Original Article
Validity of Migraine Diagnoses in Korean National Health Insurance Claims Data -
Yoonkyung Chang1,*
 , Soyoun Choi2,*
, Soyoun Choi2,* , Byung-Su Kim1
, Byung-Su Kim1 , Tae-Jin Song2
, Tae-Jin Song2
-
Headache and Pain Research 2025;26(2):154-161.
DOI: https://doi.org/10.62087/hpr.2025.0004
Published online: June 19, 2025
1Department of Neurology, Ewha Womans University Mokdong Hospital, Ewha Womans University College of Medicine, Seoul, Republic of Korea
2Department of Neurology, Ewha Womans University Seoul Hospital, Ewha Womans University College of Medicine, Seoul, Republic of Korea
- Correspondence: Tae-Jin Song, M.D., Ph.D. Department of Neurology, Ewha Womans University Seoul Hospital, Ewha Womans University College of Medicine, 260 Gonghang-daero, Gangseo-gu, Seoul 07804, Republic of Korea Tel: +82-2-6986-1672, Fax: +82-2-6986-7000, E-mail: knstar@ewha.ac.kr
- *These authors contributed equally to this study as co-first authors.
© 2025 The Korean Headache Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 3,808 Views
- 27 Download
- 1 Crossref
Abstract
-
Purpose
- Accurate case identification using administrative datasets relies on diagnostic coding, yet these codes’ accuracy for migraine remains uncertain. This study aimed to validate the diagnostic accuracy of International Statistical Classification of Diseases and Related Health Problems 10th Revision (International Classification of Diseases, ICD-10) codes for migraine, migraine without aura (MOA), and migraine with aura (MA) in the Korean National Health Insurance Service database.
-
Methods
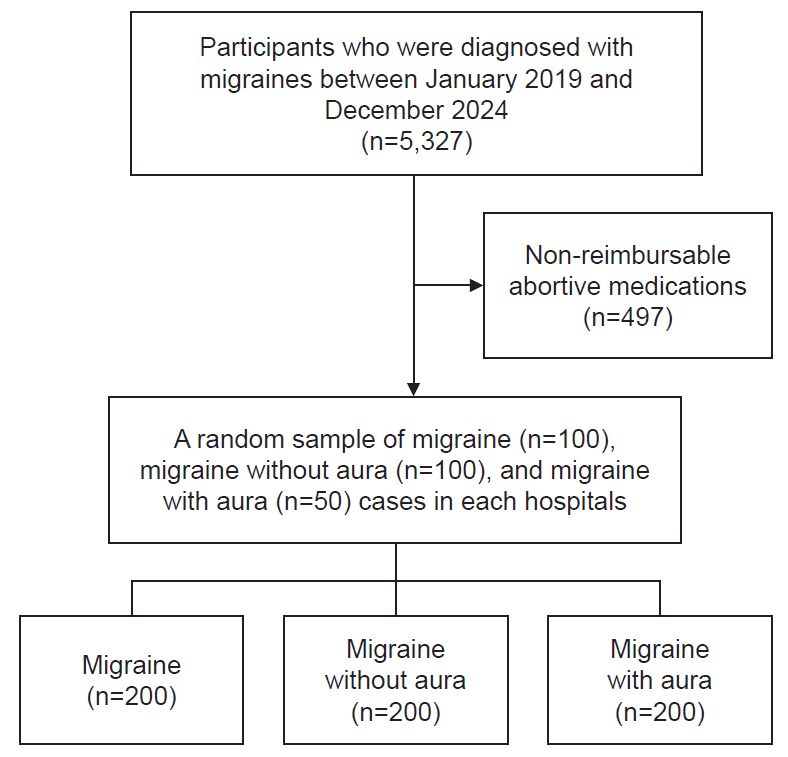
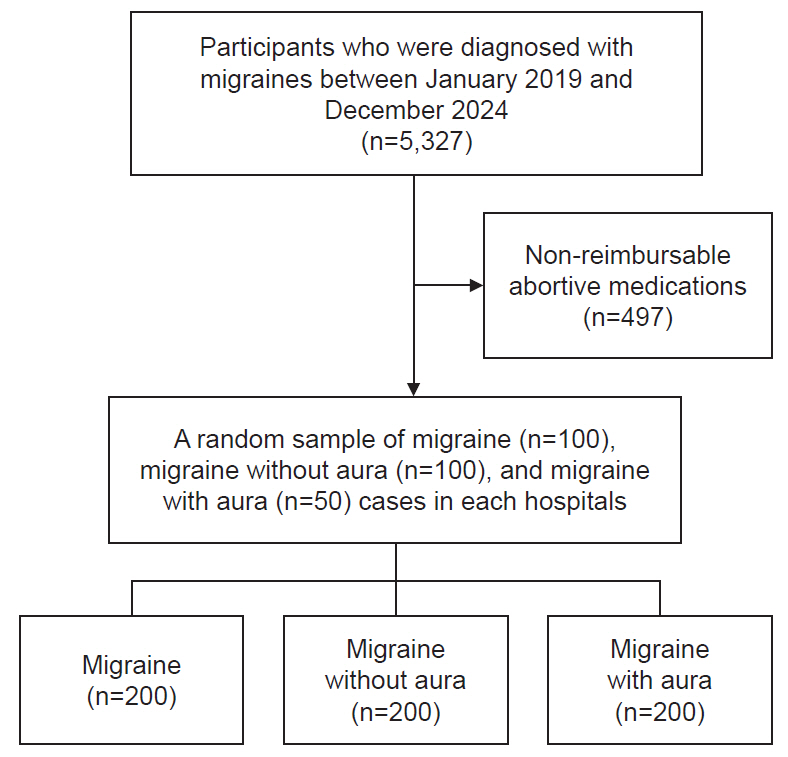
- We retrospectively reviewed the electronic medical records of 500 patients (migraine [G43.X], 200; MOA [G43.0], 200; MA [G43.1], 100) from secondary and tertiary hospitals between January 2019 and December 2024. Diagnoses confirmed by headache specialists using the International Classification of Headache Disorders, third edition served as the gold standard. Validation metrics included the positive predictive value (PPV), negative predictive value, sensitivity, specificity, and the kappa statistic. Diagnostic accuracy was assessed based on ICD-10 claim frequency and improved by combining diagnostic codes with prescriptions for migraine medications.
-
Results
- A single ICD-10 claim had a PPV of 74.00%. Accuracy improved significantly with increased claim frequency (≥3 claims: PPV, 81.14%; sensitivity, 98.61%; specificity, 28.26%), particularly when combined with medication prescriptions (≥3 claims with medication: PPV, 94.96%; sensitivity, 91.87%; specificity, 85.37%). MOA (≥3 claims with medication: PPV, 95.20%) and MA (≥3 claims with medication: PPV, 93.65%) showed similar trends. Excellent inter-rater reliability was observed (kappa, 0.806–0.951), with no significant accuracy differences between hospitals.
-
Conclusion
- Employing multiple claims and prescriptions improved the accuracy of migraine diagnoses using ICD-10 codes, supporting the use of this method in epidemiological studies and health policy decisions.
INTRODUCTION
MATERIALS AND METHODS
RESULTS
DISCUSSION
AVAILABILITY OF DATA AND MATERIAL
Upon request, the dataset for this study can be provided after consultation with the corresponding author and approval from the IRB of Ewha Womans University.
AUTHOR CONTRIBUTIONS
Conceptualization: YC, SC, BSK, TJS; Data curation: YC, SC, BSK, TJS; Formal analysis: YC, SC, BSK, TJS; Funding acquisition: TJS; Investigation: YC, SC, BSK; Methodology: YC, SC; Project administration: YC, SC, TJS; Resources: YC, SC, TJS; Software: YC, SC, TJS; Supervision: TJS; Validation: TJS; Visualization: YC, SC; Writing–original draft: YC, SC; Writing–review & editing: YC, SC, BSK, TJS.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING STATEMENT
This study was supported by a 2025 Ewha Fellow research grant from Ewha Womans University.
ACKNOWLEDGMENTS
Not applicable.
SUPPLEMENTARY MATERIAL
Supplementary Table 1.
Supplementary Table 2.
- 1. GBD 2016 Headache Collaborators. Global, regional, and national burden of migraine and tension-type headache, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2018;17:954-976.ArticlePubMedPMC
- 2. Kang S, Eum S, Chang Y, et al. Burden of neurological diseases in Asia from 1990 to 2019: a systematic analysis using the Global Burden of Disease Study data. BMJ Open 2022;12:e059548.ArticlePubMedPMC
- 3. Kim S, Park JW. Migraines in women: a focus on reproductive events and hormonal milestones. Headache Pain Res 2024;25:3-15.ArticlePDF
- 4. Gawde P, Shah H, Patel H, et al. Revisiting migraine: the evolving pathophysiology and the expanding management armamentarium. Cureus 2023;15:e34553.ArticlePubMedPMC
- 5. Pleș H, Florian IA, Timis TL, et al. Migraine: advances in the pathogenesis and treatment. Neurol Int 2023;15:1052-1105.ArticlePubMedPMC
- 6. Cho SJ, Song TJ, Chu MK. Sleep and tension-type headache. Curr Neurol Neurosci Rep 2019;19:44.ArticlePubMedPDF
- 7. Song TJ, Cho SJ, Kim WJ, Yang KI, Yun CH, Chu MK. Anxiety and depression in probable migraine: a population-based study. Cephalalgia 2017;37:845-854.ArticlePubMedPDF
- 8. Song TJ, Cho SJ, Kim WJ, Yang KI, Yun CH, Chu MK. Sex differences in prevalence, symptoms, impact, and psychiatric comorbidities in migraine and probable migraine: a population-based study. Headache 2019;59:215-223.ArticlePubMedPDF
- 9. Kalkman DN, Couturier EGM, El Bouziani A, et al. Migraine and cardiovascular disease: what cardiologists should know. Eur Heart J 2023;44:2815-2828.ArticlePubMedPDF
- 10. Blonde L, Khunti K, Harris SB, Meizinger C, Skolnik NS. Interpretation and impact of real-world clinical data for the practicing clinician. Adv Ther 2018;35:1763-1774.ArticlePubMedPMCPDF
- 11. Seong SC, Kim YY, Park SK, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open 2017;7:e016640.ArticlePubMedPMC
- 12. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol 2017;46:e15.ArticlePubMed
- 13. Choi S, Leem GH, Song TJ. Association of varicose veins with incidence risk of atrial fibrillation: a population-based cohort study. Int J Surg 2024;110:5704-5712.ArticlePubMedPMC
- 14. Park JH, Leem GH, Kim JW, Song TJ. Persisting chronic periodontal disease as a risk factor for cardiovascular disease: a nationwide population-based cohort study. J Clin Periodontol 2025;52:375-386.ArticlePubMed
- 15. Steindel SJ. International classification of diseases, 10th edition, clinical modification and procedure coding system: descriptive overview of the next generation HIPAA code sets. J Am Med Inform Assoc 2010;17:274-282.ArticlePubMedPMC
- 16. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018;38:1-211.ArticlePubMed
- 17. Kim KY, Ko HY, Bea S, Lee HJ, Shin JY, Chu MK. Treatment patterns and persistence among patients newly diagnosed with migraine in South Korea: a retrospective analysis of health claims data. J Clin Neurol 2024;20:529-536.ArticlePubMedPMCPDF
- 18. Kim BS, Chung PW, Chung JM, et al. Evidence-based recommendations on pharmacologic treatment for migraine prevention: a clinical practice guideline from the Korean Headache Society. Headache Pain Res 2025;26:5-20.ArticlePDF
- 19. Altman DG, Bland JM. Diagnostic tests 1: sensitivity and specificity. BMJ 1994;308:1552.ArticlePubMedPMC
- 20. Lee CK, Ha HJ, Oh SJ, et al. Nationwide validation study of diagnostic algorithms for inflammatory bowel disease in Korean National Health Insurance Service database. J Gastroenterol Hepatol 2020;35:760-768.ArticlePubMed
- 21. Park J, Kwon S, Choi EK, et al. Validation of diagnostic codes of major clinical outcomes in a National Health Insurance database. Int J Arrhythm 2019;20:5.ArticlePDF
- 22. Seo HJ, Oh IH, Yoon SJ. A comparison of the cancer incidence rates between the national cancer registry and insurance claims data in Korea. Asian Pac J Cancer Prev 2012;13:6163-6168.ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Toward Precision Migraine Care: Genetics, Symptoms, and Big-Data-Driven Approaches
Soo-Jin Cho
Headache and Pain Research.2025; 26(3): 171. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
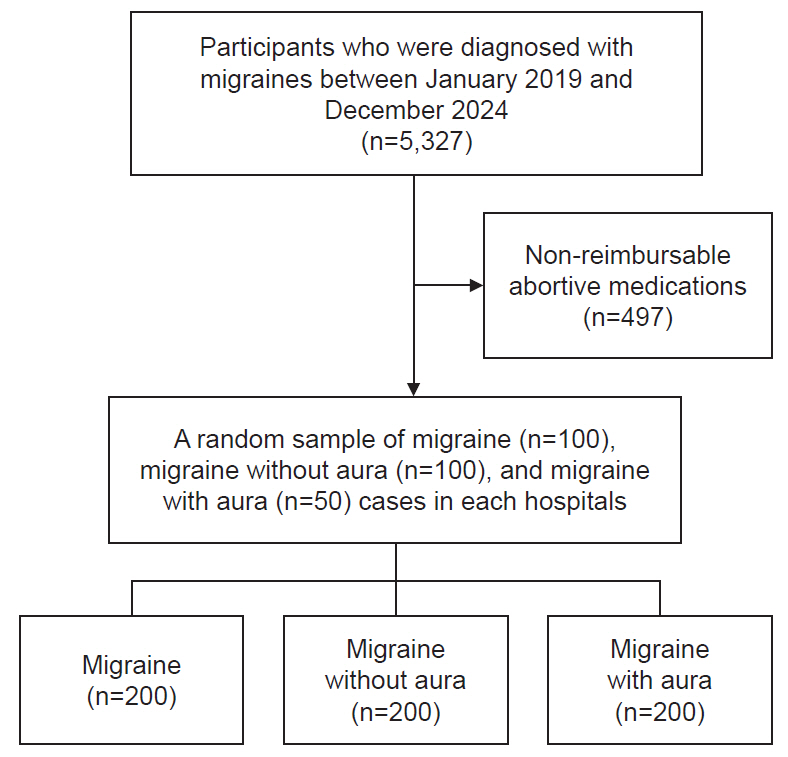
Figure 1.
| Total (n) | True positive (n) | False positive (n) | PPV (%) | NPV (%) | Error rate (%) | Sensitivity (%) | Specificity (%) | Kappa value | |
|---|---|---|---|---|---|---|---|---|---|
| Secondary hospital | |||||||||
| 1 Claim for migraine | 100 | 80 | 20 | 80.00 | - | 20.00 | - | - | - |
| 2 Claims for migraine | 98 | 79 | 17 | 82.29 | 50.00 | 18.37 | 98.75 | 5.56 | 0.806 |
| ≥3 Claims for migraine | 97 | 78 | 6 | 92.86 | 84.62 | 8.25 | 97.50 | 64.71 | 0.806 |
| 2 Claims for migraine with acute or chronic medication | 97 | 73 | 6 | 92.41 | 83.33 | 8.79 | 97.33 | 62.50 | 0.865 |
| ≥3 Claims for migraine with acute or chronic medication | 85 | 66 | 1 | 98.51 | 77.78 | 5.88 | 94.29 | 93.33 | 0.896 |
| Tertiary hospital | |||||||||
| 1 Claim for migraine | 100 | 68 | 32 | 68.00 | - | 32.00 | - | - | - |
| 2 Claims for migraine | 97 | 64 | 29 | 68.82 | 75.00 | 30.93 | 98.46 | 9.38 | 0.806 |
| ≥3 Claims for migraine | 93 | 64 | 27 | 70.33 | 100 | 28.00 | 100 | 6.90 | 0.806 |
| 2 Claims for migraine with acute or chronic medication | 88 | 58 | 27 | 68.24 | 100 | 30.68 | 100 | 10.00 | 0.865 |
| ≥3 Claims for migraine with acute or chronic medication | 80 | 47 | 5 | 90.38 | 78.57 | 13.75 | 88.68 | 80.77 | 0.896 |
| Total | |||||||||
| 1 Claim for migraine | 200 | 148 | 52 | 74.00 | - | 26.00 | - | - | - |
| ≥2 Claims for migraine | 195 | 143 | 46 | 75.66 | 66.67 | 24.62 | 98.62 | 8.00 | 0.806 |
| ≥3 Claims for migraine | 190 | 142 | 33 | 81.14 | 86.67 | 17.53 | 98.61 | 28.26 | 0.806 |
| ≥2 Claims for migraine with acute or chronic medication | 179 | 131 | 33 | 79.88 | 86.67 | 19.55 | 98.50 | 28.26 | 0.865 |
| ≥3 Claims for migraine with acute or chronic medication | 165 | 113 | 6 | 94.96 | 78.26 | 9.70 | 91.87 | 85.37 | 0.896 |
| Total (n) | True positive (n) | False positive (n) | PPV (%) | NPV (%) | Error rate (%) | Sensitivity (%) | Specificity (%) | Kappa value | |
|---|---|---|---|---|---|---|---|---|---|
| Secondary hospital | |||||||||
| 1 Claim for migraine | 100 | 80 | 20 | 80.00 | - | - | - | - | - |
| 2 Claims for migraine | 100 | 79 | 17 | 82.29 | 75.00 | 18.00 | 98.75 | 15.00 | 0.878 |
| ≥3 Claims for migraine | 100 | 78 | 6 | 92.86 | 87.50 | 8.00 | 97.50 | 70.00 | 0.912 |
| 2 Claims for migraine with acute or chronic medication | 98 | 76 | 6 | 92.68 | 81.25 | 9.18 | 96.20 | 68.42 | 0.951 |
| ≥3 claims for migraine with acute or chronic medication | 92 | 68 | 1 | 98.55 | 78.26 | 6.52 | 93.15 | 94.74 | 0.951 |
| Tertiary hospital | |||||||||
| 1 Claim for migraine | 100 | 68 | 32 | 68.00 | - | - | - | - | - |
| 2 Claims for migraine | 100 | 66 | 29 | 69.47 | 60.00 | 31.00 | 97.06 | 9.38 | 0.878 |
| ≥3 Claims for migraine | 100 | 68 | 26 | 72.34 | 100 | 26.00 | 100 | 18.75 | 0.912 |
| 2 Claims for migraine with acute or chronic medication | 92 | 62 | 25 | 71.26 | 100 | 27.17 | 100 | 16.67 | 0.951 |
| ≥3 Claims for migraine with acute or chronic medication | 89 | 51 | 5 | 91.07 | 75.76 | 14.61 | 86.44 | 83.33 | 0.951 |
| Total | |||||||||
| 1 Claim for migraine | 200 | 148 | 52 | 74.00 | - | - | - | - | - |
| ≥2 Claims for migraine | 200 | 145 | 46 | 75.92 | 66.67 | 24.50 | 97.97 | 11.54 | 0.878 |
| ≥3 Claims for migraine | 200 | 146 | 32 | 82.02 | 90.91 | 17.00 | 98.65 | 38.46 | 0.912 |
| ≥2 Claims for migraine with acute or chronic medication | 190 | 132 | 31 | 81.66 | 85.71 | 17.89 | 97.87 | 36.73 | 0.951 |
| ≥3 Claims for migraine with acute or chronic medication | 181 | 119 | 6 | 95.20 | 76.79 | 10.50 | 90.15 | 87.76 | 0.951 |
| Total (n) | True positive (n) | False positive (n) | PPV (%) | NPV (%) | Error rate (%) | Sensitivity (%) | Specificity (%) | Kappa value | |
|---|---|---|---|---|---|---|---|---|---|
| Secondary hospital | |||||||||
| 1 Claim for migraine | 50 | 39 | 11 | 78.00 | - | - | - | - | - |
| 2 Claims for migraine | 49 | 39 | 9 | 81.25 | 100 | 18.37 | 100 | 10.00 | 0.912 |
| ≥3 Claims for migraine | 48 | 38 | 3 | 92.68 | 85.71 | 8.33 | 97.44 | 66.67 | 0.951 |
| 2 Claims for migraine with acute or chronic medication | 46 | 36 | 3 | 92.31 | 85.71 | 8.70 | 97.30 | 66.67 | 0.951 |
| ≥3 Claims for migraine with acute or chronic medication | 42 | 31 | 1 | 96.88 | 70.00 | 9.52 | 91.18 | 87.50 | 0.951 |
| Tertiary hospital | |||||||||
| 1 Claim for migraine | 50 | 37 | 13 | 74.00 | - | - | - | - | - |
| 2 Claims for migraine | 48 | 35 | 11 | 76.09 | 100 | 22.92 | 100 | 15.38 | 0.912 |
| ≥3 Claims for migraine | 48 | 35 | 12 | 74.47 | 100 | 25.00 | 100 | 7.69 | 0.951 |
| 2 Claims for migraine with acute or chronic medication | 45 | 32 | 12 | 72.73 | 100 | 26.67 | 100 | 7.69 | 0.951 |
| ≥3 Claims for migraine with acute or chronic medication | 42 | 28 | 3 | 90.32 | 72.73 | 14.29 | 90.32 | 72.73 | 0.951 |
| Total | |||||||||
| 1 Claim for migraine | 100 | 76 | 24 | 76.00 | - | - | - | - | - |
| ≥2 Claims for migraine | 97 | 74 | 20 | 78.72 | 100 | 20.62 | 100 | 13.04 | 0.912 |
| ≥3 Claims for migraine | 96 | 73 | 15 | 82.95 | 87.50 | 16.67 | 98.65 | 31.82 | 0.951 |
| ≥2 Claims for migraine with acute or chronic medication | 91 | 68 | 15 | 81.93 | 87.50 | 17.58 | 98.55 | 31.82 | 0.951 |
| ≥3 Claims for migraine with acute or chronic medication | 84 | 59 | 4 | 93.65 | 71.43 | 11.90 | 90.77 | 78.95 | 0.951 |
NPV, negative predictive value; PPV, positive predictive value.
NPV, negative predictive value; PPV, positive predictive value.
NPV, negative predictive value; PPV, positive predictive value.
Table 1.
Table 2.
Table 3.
TOP
 KHS
KHS