Articles
- Page Path
- HOME > Headache Pain Res > Volume 25(2); 2024 > Article
-
Review Article
What a Neurologist Should Know about Functional Anatomy for Botulinum Toxin Injections in the Head, Face, and Neck: A Practical Perspective -
So Ra Kim1
 , Vittorio Favero2
, Vittorio Favero2 , Alec Hyung Kim3
, Alec Hyung Kim3 , SeongTaek Kim4
, SeongTaek Kim4
-
Headache and Pain Research 2024;25(2):77-85.
DOI: https://doi.org/10.62087/hpr.2024.0005
Published online: July 22, 2024
1Department of Oral Medicine, Chonnam National University Dental Hospital, Gwangju, Republic of Korea
2Department of Neuroscience, University of Padova, Padova, Italy
3TMJ & Orofacial Pain Center, Los Angeles, CA, USA
4Department of Orofacial Pain and Oral Medicine, Yonsei University College of Dentistry, Seoul, Republic of Korea
- Correspondence: SeongTaek Kim, DDS, Ph.D. Department of Orofacial Pain and Oral Medicine, Yonsei University College of Dentistry, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Republic of Korea Tel: +82-2-2228-3110, Fax: +82-2-393-5673, E-mail: k8756050@yuhs.ac
• Received: March 19, 2024 • Revised: April 14, 2024 • Accepted: May 2, 2024
© 2024 The Korean Headache Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 9,680 Views
- 165 Download
- 1 Crossref
Figure & Data
References
Citations
Citations to this article as recorded by 

- When Should Headache Specialists Hold a Needle? The Role of Botulinum Toxin Injections and Occipital Nerve Blocks
Soo-Jin Cho
Headache and Pain Research.2024; 25(2): 73. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
What a Neurologist Should Know about Functional Anatomy for Botulinum Toxin Injections in the Head, Face, and Neck: A Practical Perspective
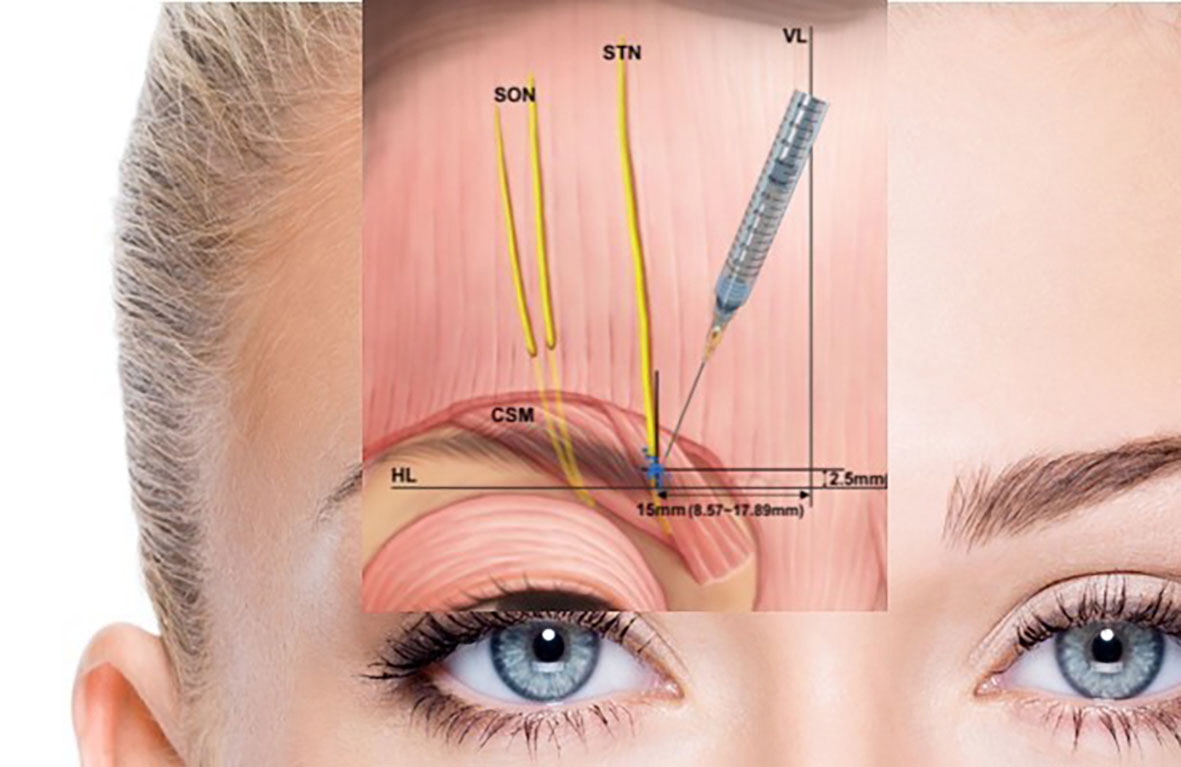
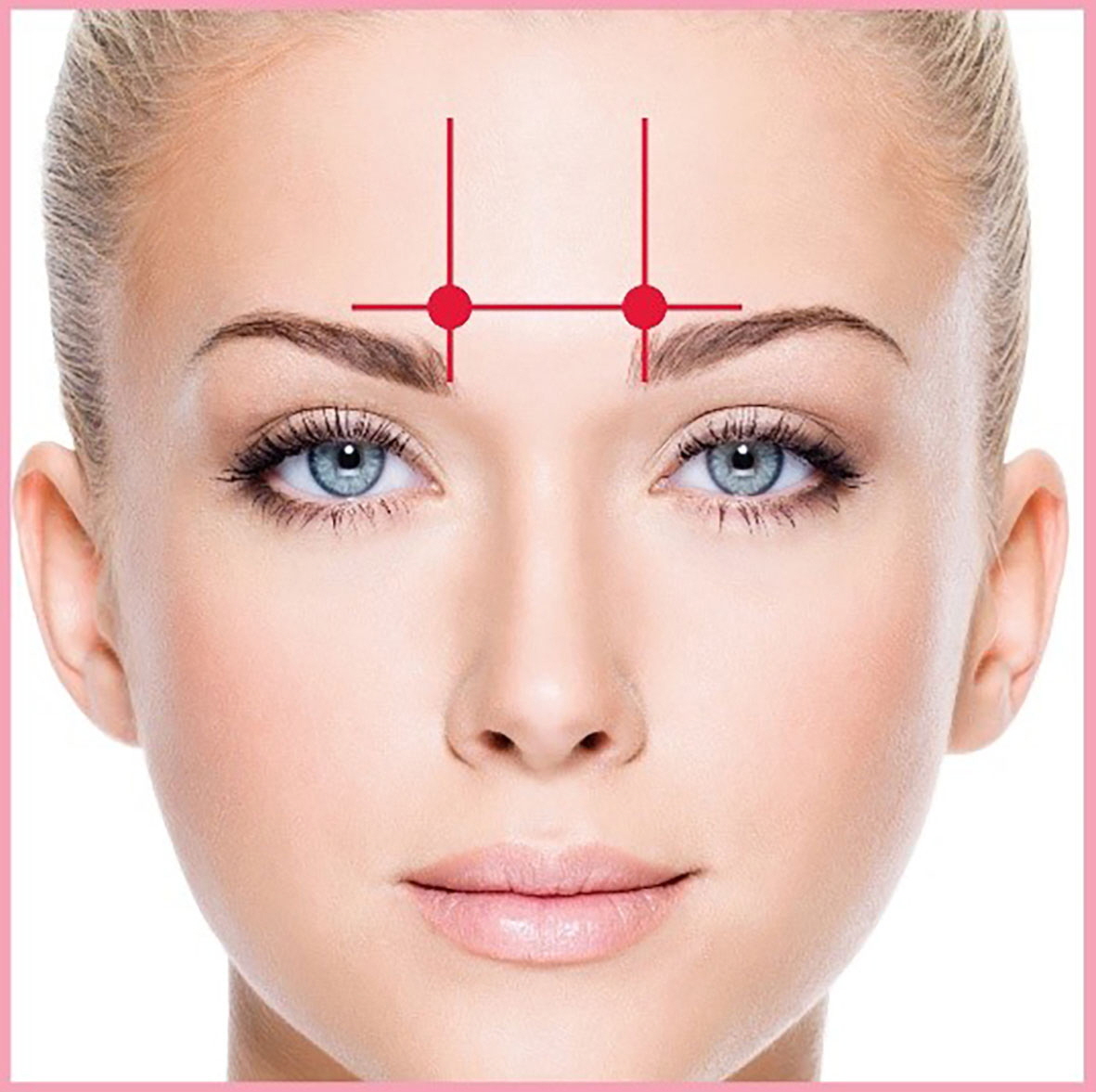
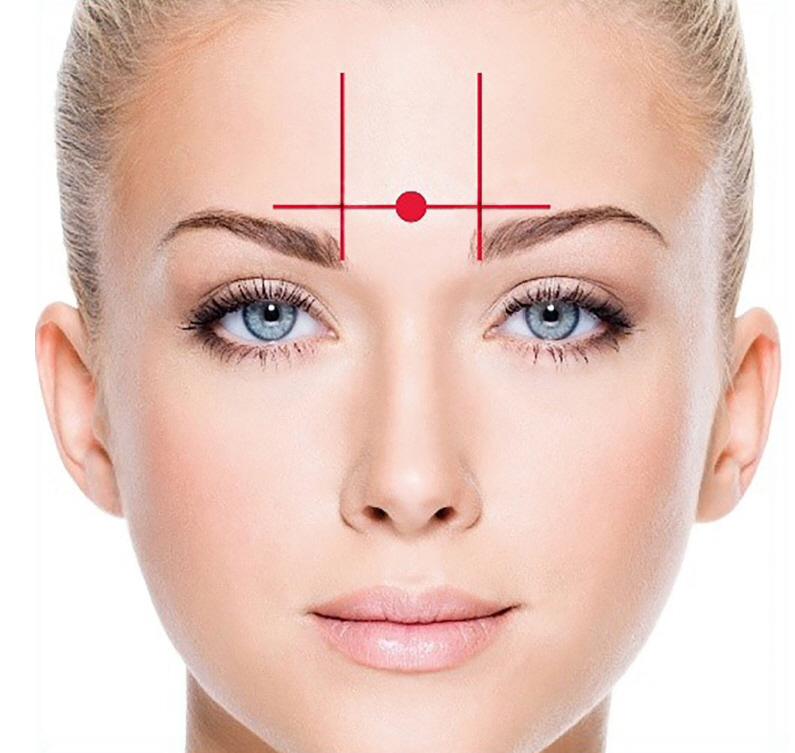
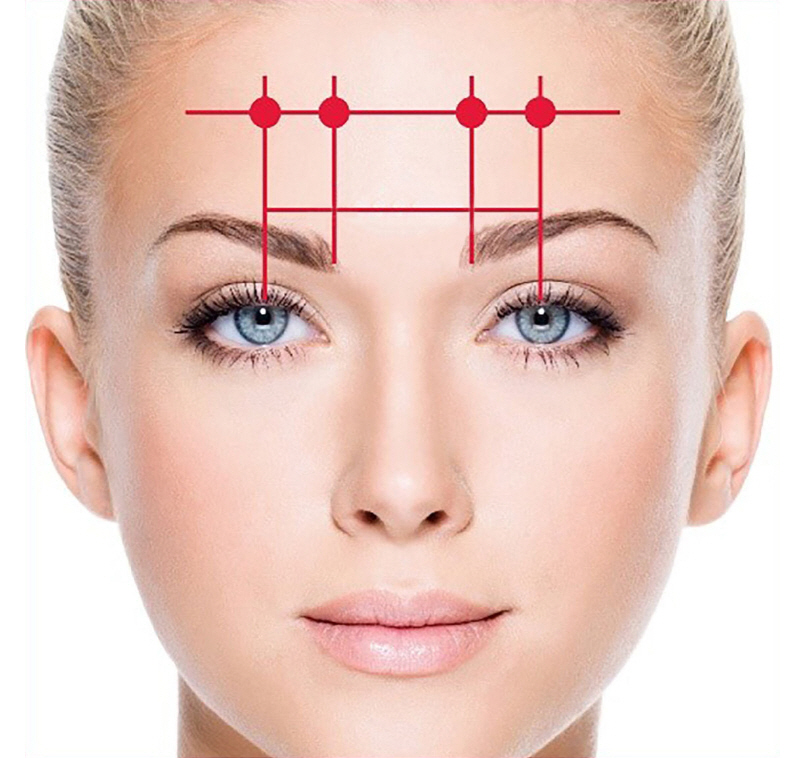


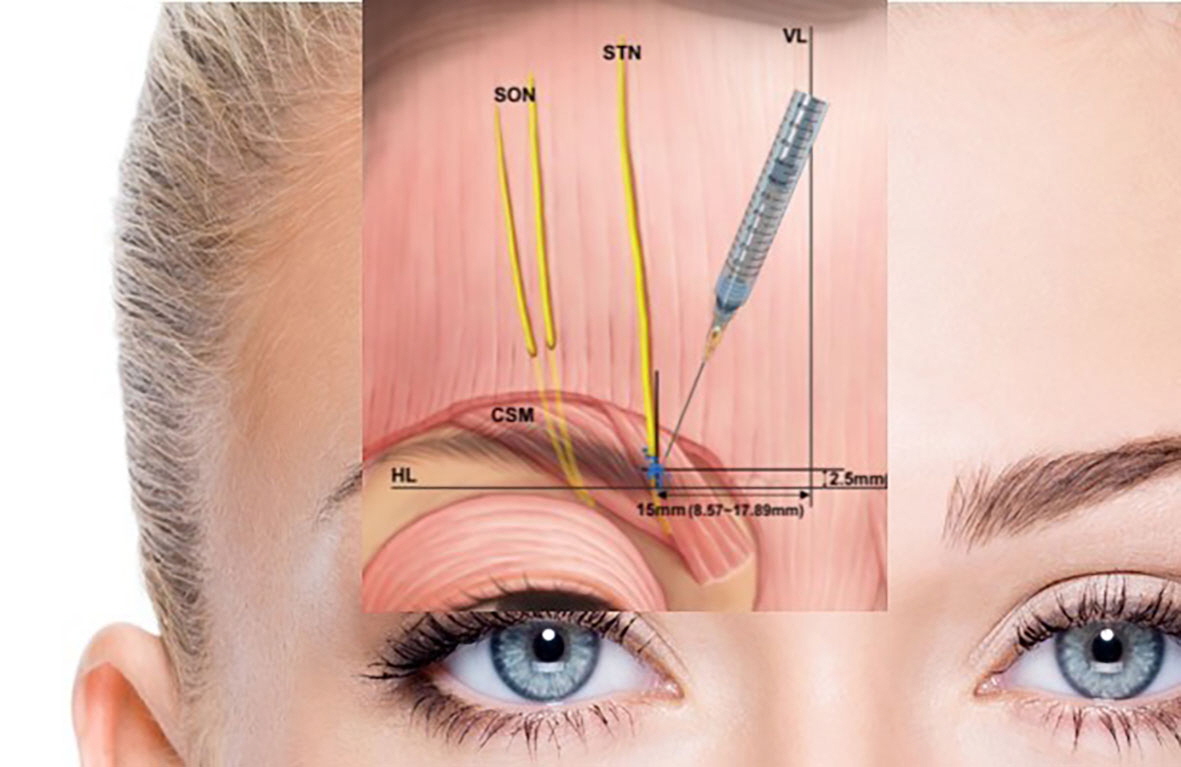
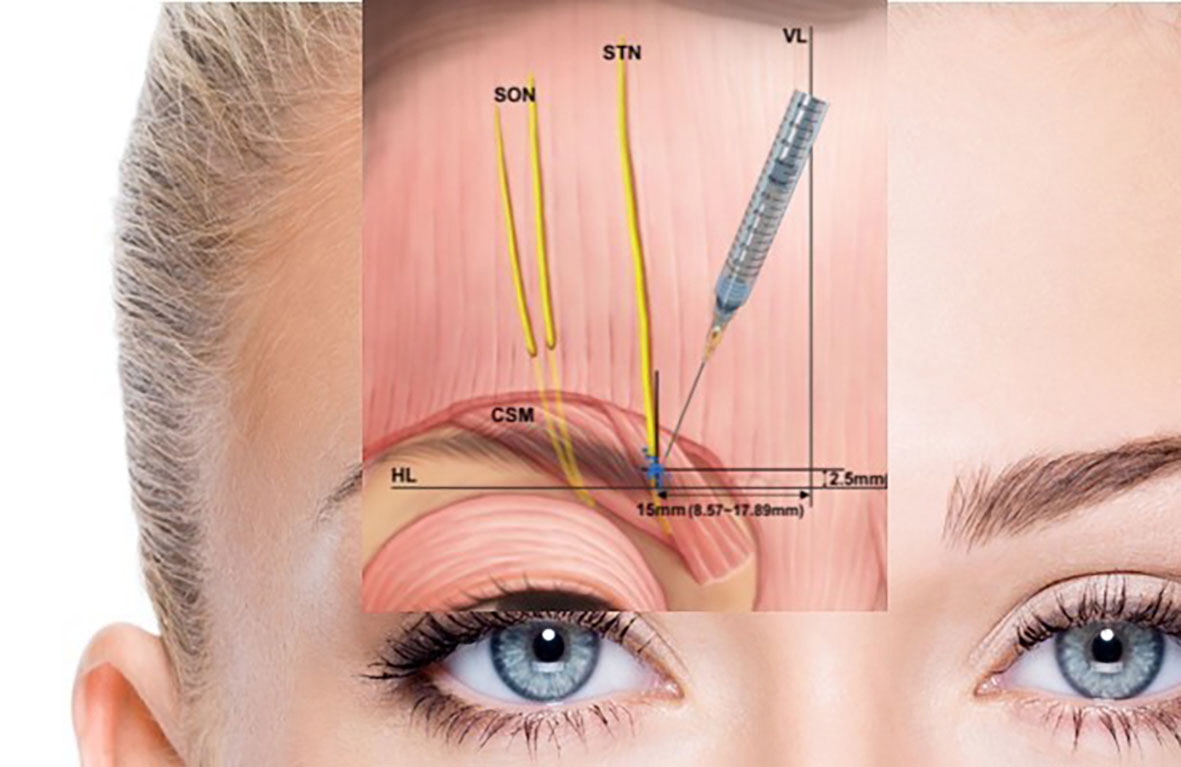
Figure 1. Distributions of the supratrochlear nerve (STN), supraorbital nerve (SON), and corrugator supercilii muscle (CSM). A previous study measured the point where the SON entered the CSM and the distance between the SON and the STN. The entry point of the STN into the CSM was found to be 16.4±4.0 mm lateral to the midsagittal line and 2.3±3.9 mm superior to the supraorbital margin. When the STN emerged separately from the orbit, it was situated 7.5±2.3 mm medial to the SON at the level of the supraorbital margin.24 Chronic migraines can be relieved by injecting botulinum toxin at the location indicated by the blue dot.VL, vertical baseline; HL, horizontal baseline.
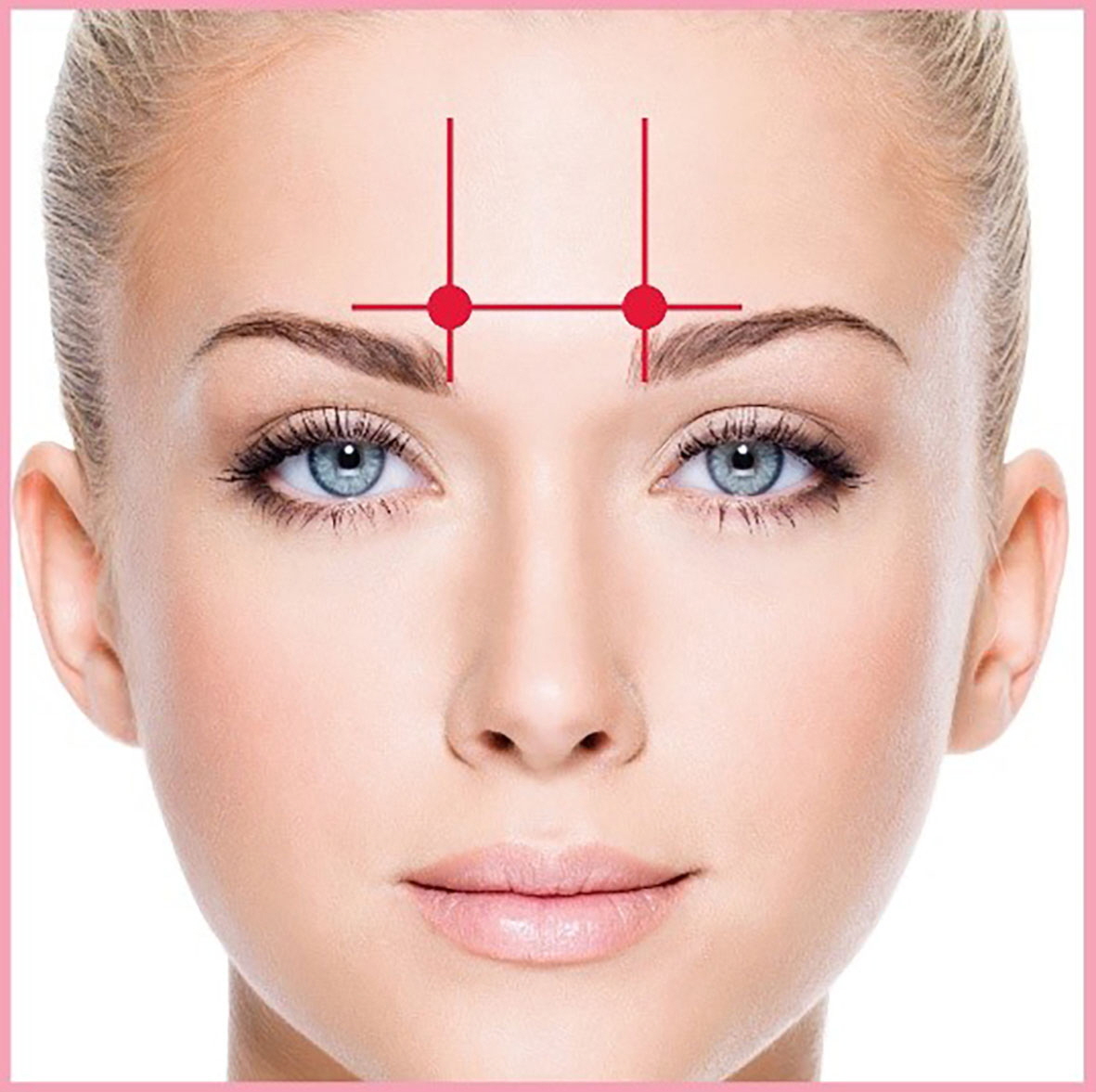
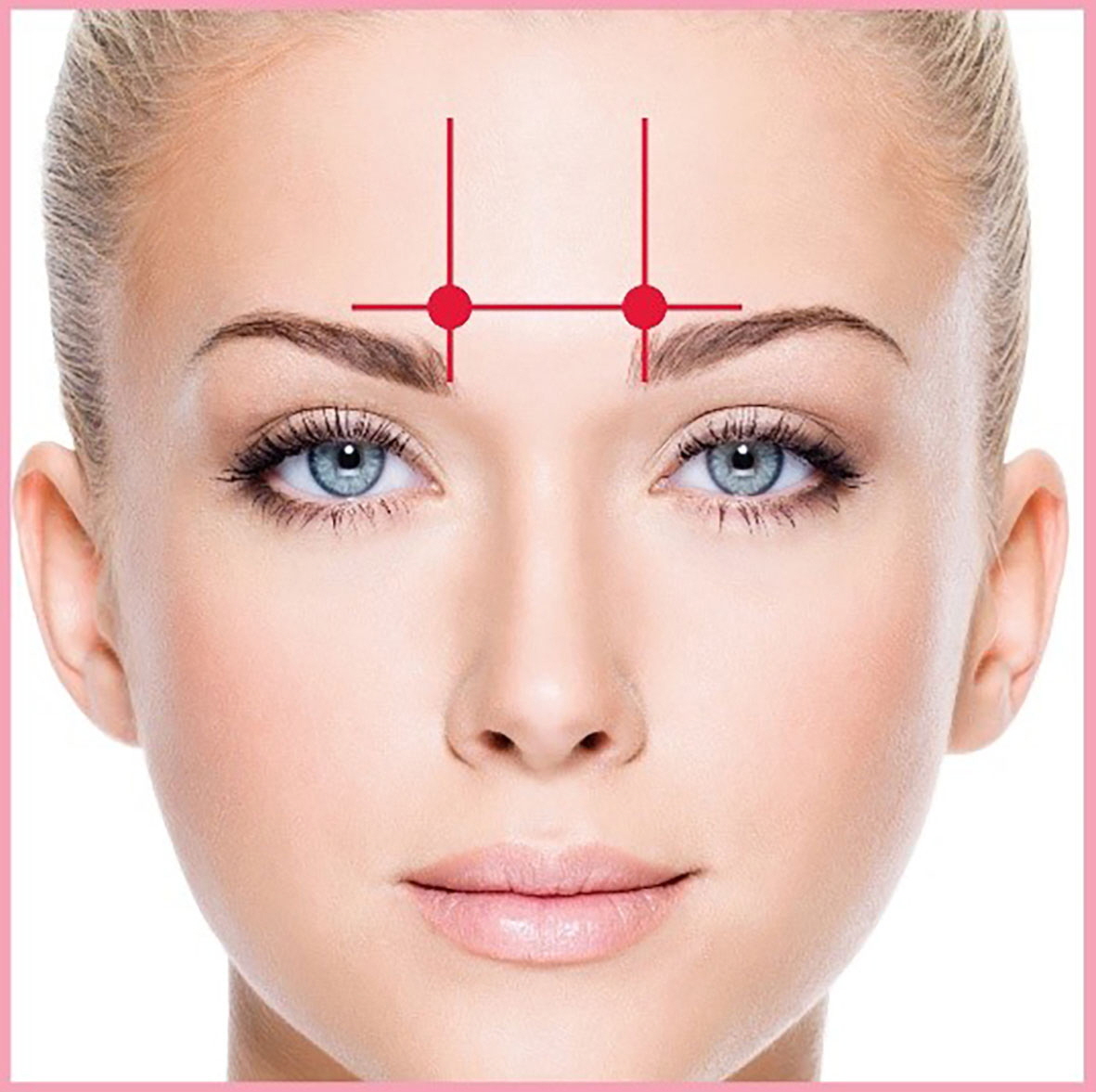
Figure 2. Corrugator muscle injection. Adapted from the book of Kim ST et al. (Dental Wisdom; 2018) with permission of copyright holder.26
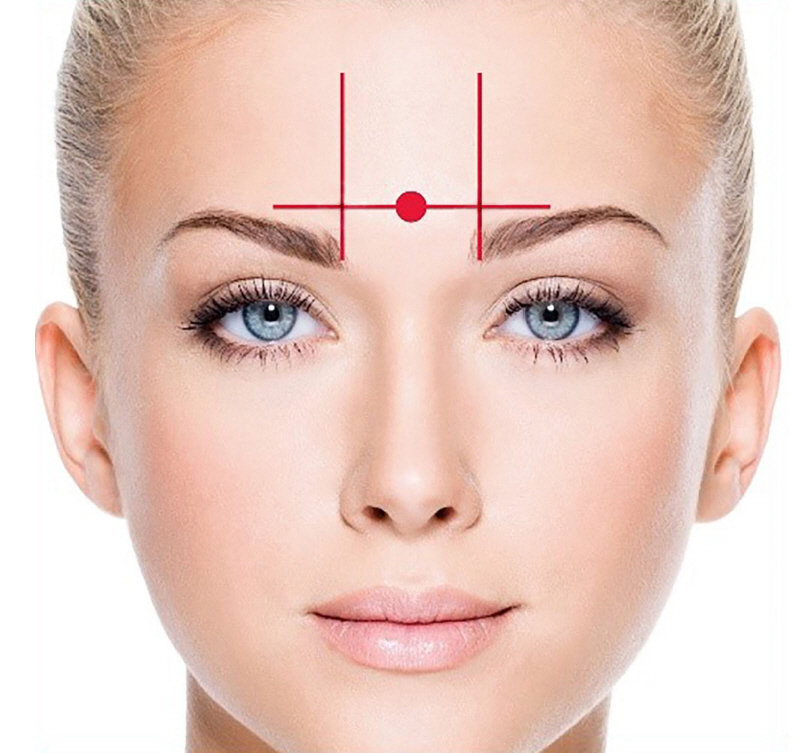
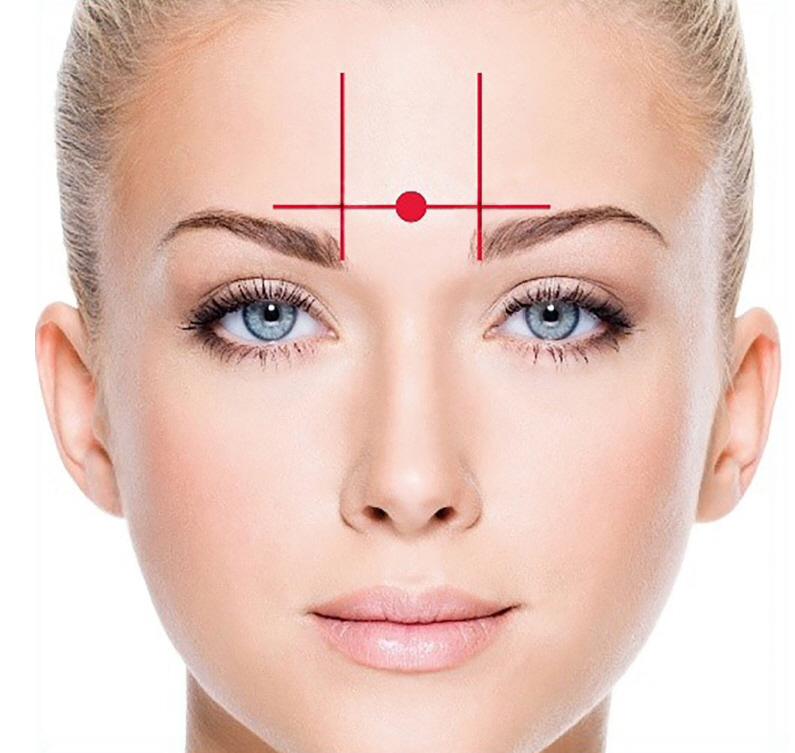
Figure 3. Procerus muscle injection. Adapted from the book of Kim ST et al. (Dental Wisdom; 2018) with permission of copyright holder.26
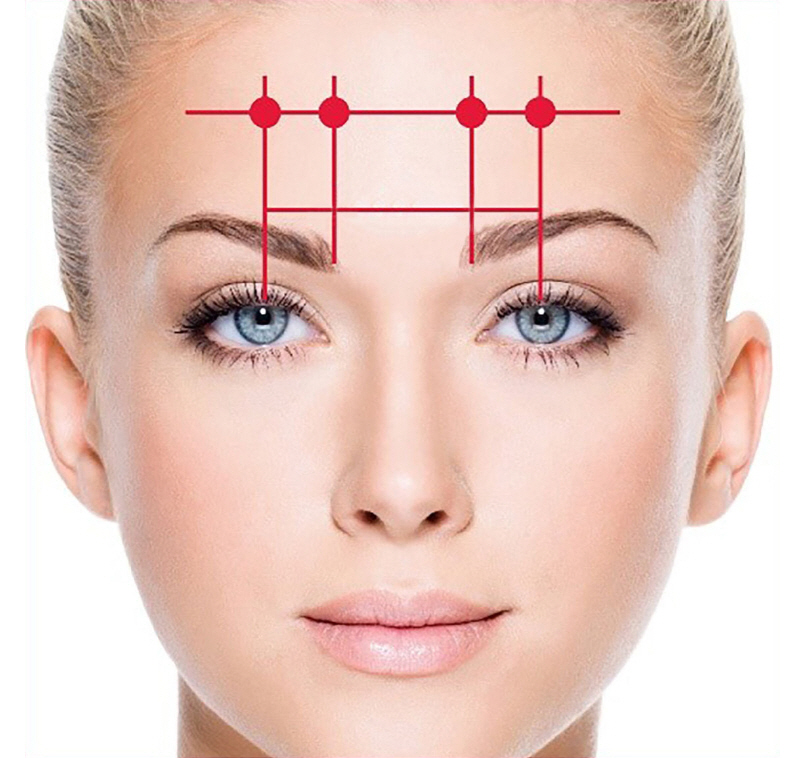
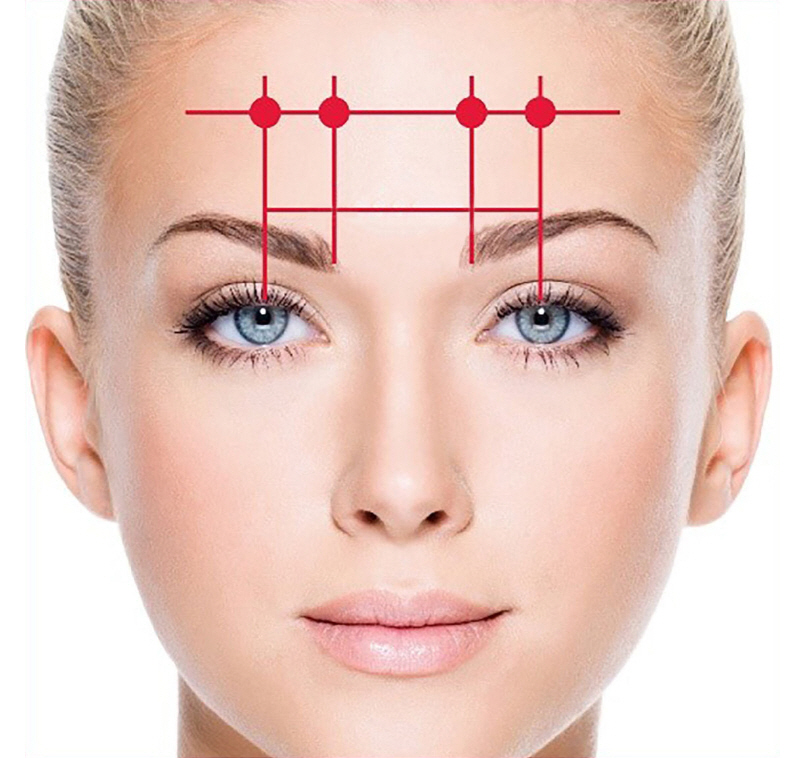
Figure 4. Frontalis muscle injection. Adapted from the book of Kim ST et al. (Dental Wisdom; 2018) with permission of copyright holder.26
Figure 5. Mephisto sign development. (A) Before botulinum toxin A (BoNT-A) injection: photograph of the patient’s frontal view before BoNT-A injection, showing normal eyebrow alignment. (B) Two weeks after the BoNT-A injection: photograph of the same patient’s frontal view two weeks after the BoNT-A injection, demonstrating the development of the Mephisto sign, characterized by the outer end of the eyebrow positioned higher than the inner end, potentially creating an intimidating impression. Adapted from the book of Kim ST et al. (Dental Wisdom; 2018) with permission of copyright holder.26
Figure 6. Superimposed nerve distributions of the auriculotemporal nerve in 16 cadavers. The nerve endings may be proposed as target injection points.26,30
Figure 7. Temporalis muscle injection. The sites corresponding to injection methods I1, I2, I3, and I4 are indicated on the following temporalis muscle structures: I1, Injection 1; I2, Injection 2; I3, Injection 3; I4: Injection 4.26
Figure 8. The great occipital nerve (GON, yellow line) is located at the third point of the virtual line, connecting the external occipital protuberance (inion) and the mastoid process (white dots). The injection sites are as follows: at the midpoint(<-middle point) of the virtual line connecting the mastoid process and inion, a point in the shape of an inverted triangle set around 3 cm from the first site and two other points that constitute the vertices of the inverted triangle. Finally, botulinum toxin (BoNT) was injected into three points (red dots) around GON, where 5 U of BoNT was administered at each point.32
Figure 9. Occipitalis muscle injection. The sites corresponding to injection methods I1, I2, and I3 are indicated on the following occipitalis muscle structures: I1, injection 1; I2, injection 2; I3, injection 3.32
Figure 10. Cervical paraspinal muscle injection. Adapted from the book of Kim ST et al. (Dental Wisdom; 2018) with permission of copyright holder.26
Figure 1.
Figure 2.
Figure 3.
Figure 4.
Figure 5.
Figure 6.
Figure 7.
Figure 8.
Figure 9.
Figure 10.
What a Neurologist Should Know about Functional Anatomy for Botulinum Toxin Injections in the Head, Face, and Neck: A Practical Perspective
TOP
 KHS
KHS