Articles
- Page Path
- HOME > Headache Pain Res > Volume 25(2); 2024 > Article
-
Review Article
Understanding the Connection between the Glymphatic System and Migraine: A Systematic Review -
Myoung-Jin Cha1
 , Kyung Wook Kang2
, Kyung Wook Kang2 , Jung-won Shin3
, Jung-won Shin3 , Hosung Kim4
, Hosung Kim4 , Jiyoung Kim5
, Jiyoung Kim5
-
Headache and Pain Research 2024;25(2):86-95.
DOI: https://doi.org/10.62087/hpr.2024.0014
Published online: July 31, 2024
1Department of Neurology, National Police Hospital, Seoul, Republic of Korea
2Department of Neurology, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Republic of Korea
3Department of Neurology and Memory Center, CHA Bundang Medical Center, CHA University, Seongnam, Republic of Korea
4USC Mark and Mary Stevens Neuroimaging and Informatics Institute, Keck School of Medicine of USC, University of Southern California, Los Angeles, CA, USA
5Department of Neurology and Biomedical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Republic of Korea
- Correspondence: Jiyoung Kim, M.D., Ph.D. Department of Neurology and Biomedical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, 179 Gudeok-ro, Seo-gu, Busan 49241, Republic of Korea Tel: +82-51-240-7311, Fax: +82-51-254-7317, E-mail: bijoukim78@gmail.com
© 2024 The Korean Headache Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 7,843 Views
- 146 Download
- 2 Crossref
Abstract
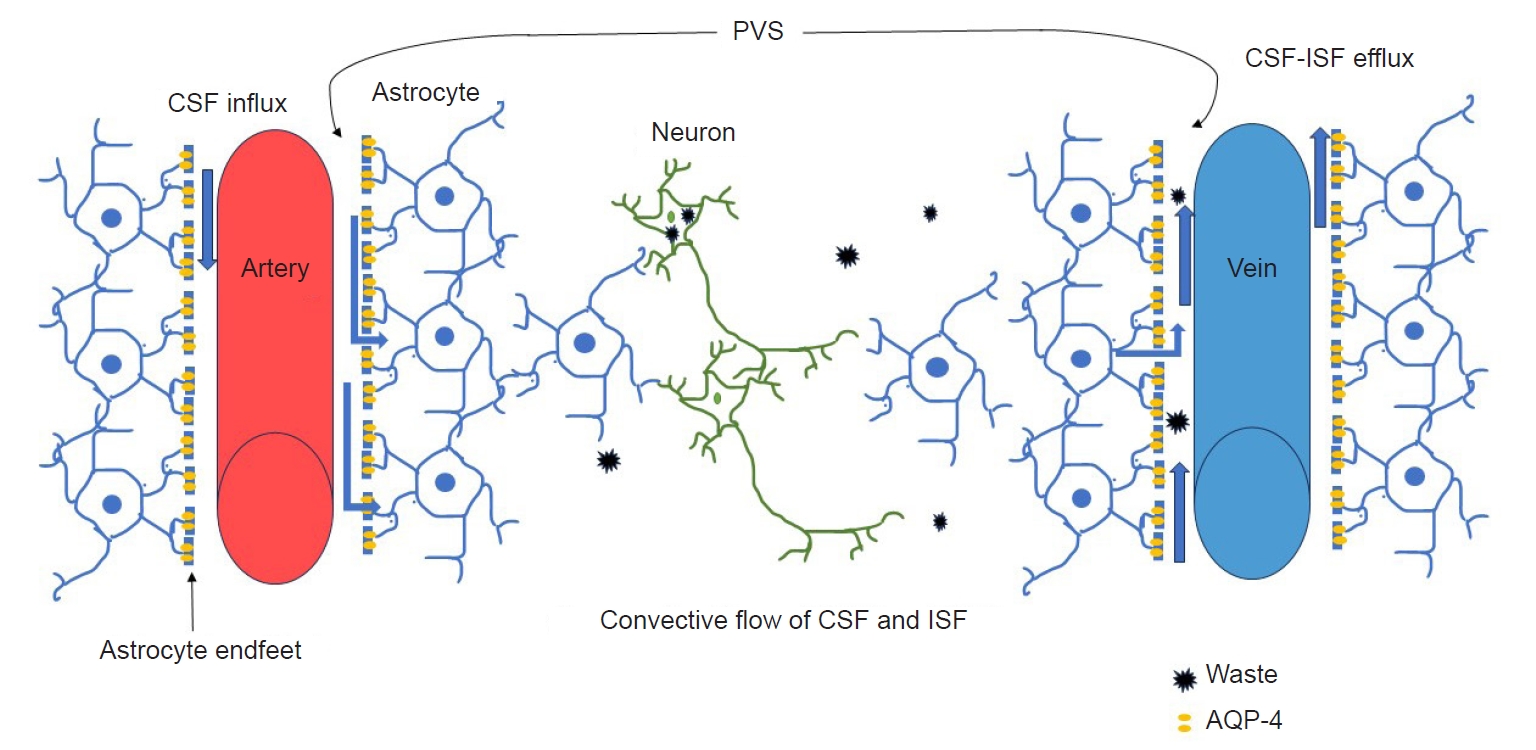
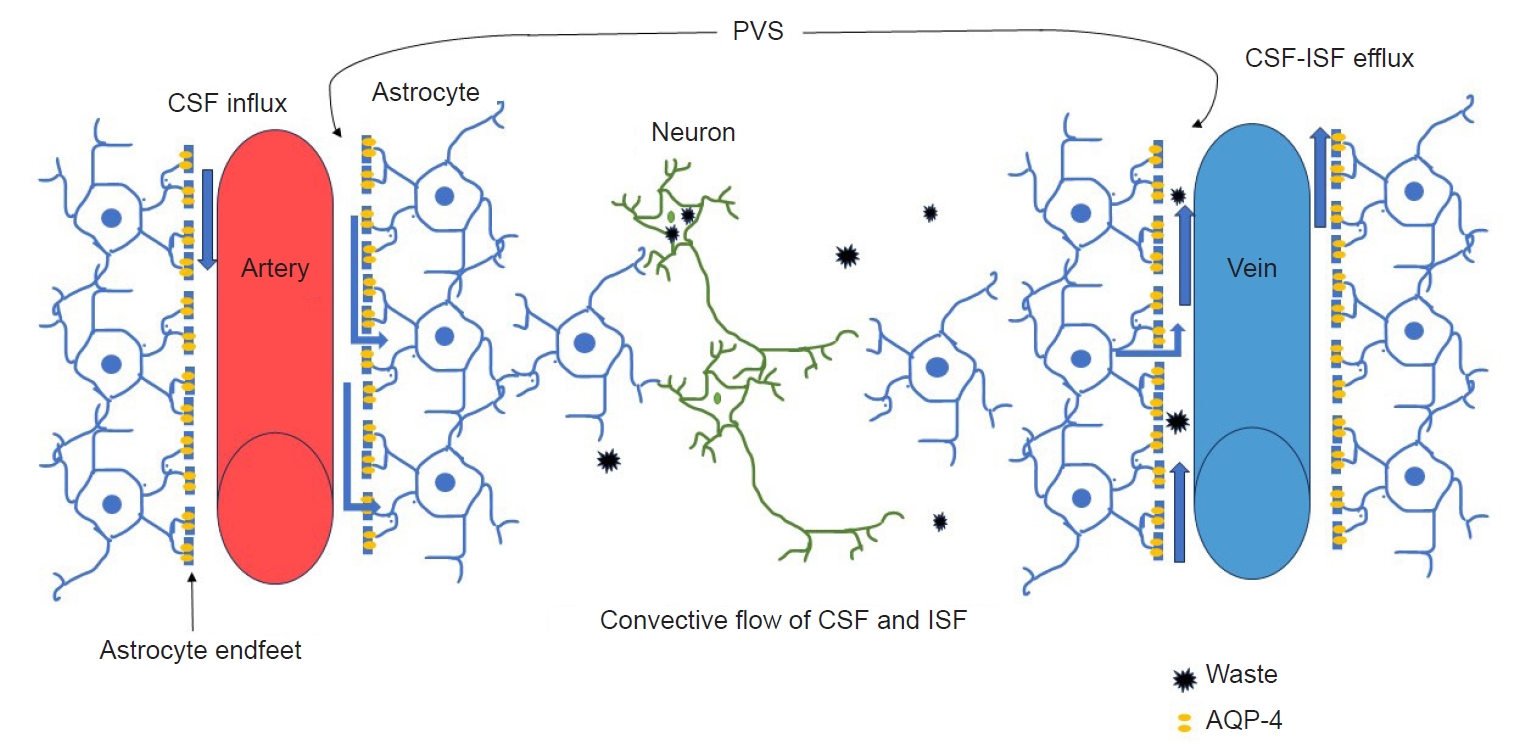
- The glymphatic system is a brain-wide perivascular pathway that functions similarly to the lymphatic system in the periphery of the body, playing a crucial role in removing waste from the brain. Although impaired glymphatic function has a well-known relationship with neurodegenerative diseases through abnormal protein accumulation, it is also associated with migraine. While still in its nascent phase, research on the glymphatic system in migraine patients is gradually increasing. This systematic literature review focuses on studies investigating the glymphatic system in migraineurs. Furthermore, it examines the methods used to evaluate the glymphatic system in these studies and their main findings.
INTRODUCTION
METHODS
RESULTS
CONCLUSION
AVAILABILITY OF DATA AND MATERIAL
Not applicable.
AUTHOR CONTRIBUTIONS
Conceptualization: JK; Data curation: MJC, JK; Formal analysis: MJC, JK; Funding acquisition: JK; Investigation: MJC, JK; Methodology: MJC, JK; Writing–original draft: MJC, JK; Writing–review and editing: MJC, KWK, JWS, HK, JK.
CONFLICT OF INTEREST
Jiyoung Kim is the editor of Headache and Pain Research and was not involved in the review process of this article. All authors have no other conflicts of interest to declare.
FUNDING STATEMENT
This study was supported by the 2023 overseas training grant from Pusan National University Hospital.
ACKNOWLEDGMENTS
Not applicable.
| Study | Location | Study design | Participants (n) | Diagnostic criteria | Age (yr)* | Study including only children† | Female/male ratio | GS assessment tool | Main outcome |
|---|---|---|---|---|---|---|---|---|---|
| Zhang et al. (2024) [36] | China | Case-control study | Migraine (48) | ICHD-3 | Migraine: 31.0 (25.5–34.0) | NA | 1.7:1 | Visual inspection of MRI | Migraine with aura was negatively correlated with the number of VRS in basal ganglia. |
| TTH (32) | TTH: 32.5 (27.5–35.5) | Visual rating scale (Potter et al. [22], (2015); https://www.ed.ac.uk/files/imports/fileManager/epvs-rating-scale-user-guide.Pdf) | Education level and migraine frequency were correlated with the number of VRS. | ||||||
| HC (49) | HC: 32.0 (24.0–37.0) | ||||||||
| Zhang et al. (2023) [30] | China | Cross-sectional study | EM (32) | ICHD-3 | EM: 34.8±15.4 | NA | 1.9:1 | DTI-ALPS index | CM had a higher DTI-ALPS index in the right hemisphere than EM and HC. |
| CM (24) | CM: 34.8±16.8 | ||||||||
| HC (41) | HC: 36.0±10.9 | ||||||||
| Jeon et al. (2023) [39]‡ | Korea | Cross-sectional study | Migraine (46) | ICHD-3 or earlier | UN | Only children | UN | Visual inspection of MRI | Dilatated PVS was the most common finding in the migraine and non-migraine headache groups. |
| Non-migraine (60) | |||||||||
| Ornello et al. (2023) [35] | Italy | Cross-sectional study | EM and CM (147) | ICHD-3 | EM and CM: 45 (36–50) | NA | 4.4:1 | DTI-ALPS index | White matter hyperintensity was not associated with an impairment in the glymphatic system in patients with migraine. |
| Yuan et al. (2023) [31] | China | Case-control study | EM (59) | ICHD-3 | EM: 39 (32–43) | NA | 2.4:1 | Visual inspection of MRI | Migraineurs had a significantly higher prevalence of high-grade enlarged PVS in centrum semiovale and midbrain than HC. |
| CM (115) | CM: 42 (33–48) | Visual rating scale (Potter et al. [22] (2015); https://www.ed.ac.uk/files/imports/fileManager/epvs-rating-scale-user-guide.Pdf) | |||||||
| HC (57) | HC: 41 (30–47) | ||||||||
| Wu et al. (2024) [32] | Taiwan | Cross-sectional study | EM (73) | ICHD-3 | EM: 37.4±10.2 | NA | 3.7:1 | DTI-ALPS index | The DTI-ALPS index was lower in CM than in EM and HC. |
| CM (39) | CM: 36.2±11.5 | Dynamic contrast-enhanced MRI for meningeal lymphatic vessels. | |||||||
| HC (63) | HC: 39.7±8.0 | ||||||||
| Lee et al. (2022) [37] | Korea | Cross-sectional study | MA (20) | ICHD-3 | MA: 36.0±12.9 | NA | 3.9:1 | DTI-ALPS index | The DTI-ALPS index did not differ between migraine patients and HC. |
| MO (72) | MO: 38.4±11.3 | ||||||||
| HC (80) | HC: 37.8±11.7 | ||||||||
| Husøy et al. (2016) [38] | Norway | Cross sectional and longitudinal study | Total (1,006) | ICHD-2 | Total range: 50–66 | NA | UN | Visual inspection and counting of visible PVS | In the cross-sectional analysis, fewer PVS were observed in migraine without aura. However, in the longitudinal analysis, there was no significant association between the number of PVS and headache, including migraine. |
| Lewis et al. (2000) [40] | United States | Cross-sectional study | Total (302) | ICHD-1-R§ | Total range: 6–18 | Only children | UN | Visual inspection of CT and MRI | Among 42 migraine patients undergoing CT scans, dilated VRS were observed in one subject. |
| Migraine (107) | |||||||||
| Schick et al. (1999) [41] | Austria | Case-control study | Migraine (31 children) | ICHD-1 | Range: 3–14 (children) | Only children (in group of migraine, TTH and headache-free children) | 1.1 (in group of migraine and TTH) | Visual inspection of MRI | The prevalence of VRS in childhood migraine was higher than in those with TTH, headache-free children, or adults with migraine. |
| TTH (27 children) | 22–55 (adults) | ||||||||
| Controls (30 headache-free children) | |||||||||
| Controls (30 migraine adult) |
GS, glymphatic system; TTH, tension-type headache; HC, healthy controls; ICHD, International Classification of Headache Disorders; NA, not applicable; MRI, magnetic resonance imaging; VRS, Virchow-Robin spaces; EM, episodic migraine; CM, chronic migraine; DTI-ALPS, diffusion tensor image analysis along the perivascular spaces; PVS, perivascular spaces; MA, migraine with aura; MO, migraine without aura; UN, uncertain; CT, computed tomography.
*Age is reported as median (interquartile range), mean±standard deviation, or range only. †A child is 18 years of age or younger. ‡The subgroup analysis results are exclusively associated with the glymphatic system, making the demographic characteristics of the participants unclear. §ICHD-1-R was proposed as a modification based on the ICHD-1.
- 1. Steiner TJ, Stovner LJ. Global epidemiology of migraine and its implications for public health and health policy. Nat Rev Neurol 2023;19:109-117.ArticlePubMedPDF
- 2. Kim KM, Cho SJ, Shin HJ, et al. Prevalence, disability, and management patterns of migraine in Korea: nationwide survey data from 2009 and 2018. J Clin Neurol 2021;17:77-85.ArticlePubMedPMCPDF
- 3. Seo JG. Menstrual migraine: a review of current research and clinical challenges. Headache Pain Res 2024;25:16-23.ArticlePDF
- 4. Kim S, Park JW. Migraines in women: a focus on reproductive events and hormonal milestones. Headache Pain Res 2024;25:3-15.ArticlePDF
- 5. Graham JR, Wolff HG. Mechanism of migraine headache and action of ergotamine tartrate. Arch NeurPsych 1938;39:737-763.Article
- 6. Biscetti L, Cresta E, Cupini LM, Calabresi P, Sarchielli P. The putative role of neuroinflammation in the complex pathophysiology of migraine: from bench to bedside. Neurobiol Dis 2023;180:106072.ArticlePubMed
- 7. Moskowitz MA. The neurobiology of vascular head pain. Ann Neurol 1984;16:157-168.ArticlePubMed
- 8. Bohr T, Hjorth PG, Holst SC, et al. The glymphatic system: current understanding and modeling. iScience 2022;25:104987.ArticlePubMedPMC
- 9. Mestre H, Verma N, Greene TD, et al. Periarteriolar spaces modulate cerebrospinal fluid transport into brain and demonstrate altered morphology in aging and Alzheimer’s disease. Nat Commun 2022;13:3897.ArticlePubMedPMCPDF
- 10. Wardlaw JM, Benveniste H, Nedergaard M, et al. Perivascular spaces in the brain: anatomy, physiology and pathology. Nat Rev Neurol 2020;16:137-153.ArticlePubMedPDF
- 11. Angeli V, Lim HY. Biomechanical control of lymphatic vessel physiology and functions. Cell Mol Immunol 2023;20:1051-1062.ArticlePubMedPMCPDF
- 12. Breslin JW, Yang Y, Scallan JP, Sweat RS, Adderley SP, Murfee WL. Lymphatic vessel network structure and physiology. Compr Physiol 2018;9:207-299.ArticlePubMedPMCPDF
- 13. Nedergaard M. Garbage truck of the brain. Science 2013;340:1529-1530.ArticlePubMedPMC
- 14. Gouveia-Freitas K, Bastos-Leite AJ. Perivascular spaces and brain waste clearance systems: relevance for neurodegenerative and cerebrovascular pathology. Neuroradiology 2021;63:1581-1597.ArticlePubMedPMCPDF
- 15. Cai Y, Zhang Y, Leng S, et al. The relationship between inflammation, impaired glymphatic system, and neurodegenerative disorders: a vicious cycle. Neurobiol Dis 2024;192:106426.ArticlePubMed
- 16. Jeong SH, Cha J, Park M, et al. Association of enlarged perivascular spaces with amyloid burden and cognitive decline in Alzheimer disease continuum. Neurology 2022;99:e1791-e1802.ArticlePubMed
- 17. Bae YJ, Kim JM, Choi BS, et al. Glymphatic function assessment in Parkinson’s disease using diffusion tensor image analysis along the perivascular space. Parkinsonism Relat Disord 2023;114:105767.ArticlePubMed
- 18. Park KM, Kim KT, Lee DA, Motamedi GK, Cho YW. Glymphatic system dysfunction in restless legs syndrome: evidenced by diffusion tensor imaging along the perivascular space. Sleep 2023;46:zsad239.ArticlePubMedPDF
- 19. Schain AJ, Melo-Carrillo A, Strassman AM, Burstein R. Cortical spreading depression closes paravascular space and impairs glymphatic flow: implications for migraine headache. J Neurosci 2017;37:2904-2915.ArticlePubMedPMC
- 20. Zhang J, Liu S, Wu Y, et al. Enlarged perivascular space and index for diffusivity along the perivascular space as emerging neuroimaging biomarkers of neurological diseases. Cell Mol Neurobiol 2023;44:14.ArticlePubMedPDF
- 21. Potter GM, Doubal FN, Jackson CA, et al. Enlarged perivascular spaces and cerebral small vessel disease. Int J Stroke 2015;10:376-381.ArticlePubMedPMCPDF
- 22. Taoka T, Masutani Y, Kawai H, et al. Evaluation of glymphatic system activity with the diffusion MR technique: diffusion tensor image analysis along the perivascular space (DTI-ALPS) in Alzheimer’s disease cases. Jpn J Radiol 2017;35:172-178.ArticlePubMedPDF
- 23. Mestre H, Kostrikov S, Mehta RI, Nedergaard M. Perivascular spaces, glymphatic dysfunction, and small vessel disease. Clin Sci (Lond) 2017;131:2257-2274.ArticlePubMedPMCPDF
- 24. Chen W, Song X, Zhang Y; Alzheimer’s Disease Neuroimaging Initiative. Assessment of the Virchow-Robin spaces in Alzheimer disease, mild cognitive impairment, and normal aging, using high-field MR imaging. AJNR Am J Neuroradiol 2011;32:1490-1495.ArticlePubMedPMC
- 25. Shen T, Yue Y, Zhao S, et al. The role of brain perivascular space burden in early-stage Parkinson’s disease. NPJ Parkinsons Dis 2021;7:12.ArticlePubMedPMCPDF
- 26. Zhang Y, Zhang R, Ye Y, et al. The influence of demographics and vascular risk factors on glymphatic function measured by diffusion along perivascular space. Front Aging Neurosci 2021;13:693787.ArticlePubMedPMC
- 27. Shen T, Yue Y, Ba F, et al. Diffusion along perivascular spaces as marker for impairment of glymphatic system in Parkinson’s disease. NPJ Parkinsons Dis 2022;8:174.ArticlePubMedPMCPDF
- 28. Carotenuto A, Cacciaguerra L, Pagani E, Preziosa P, Filippi M, Rocca MA. Glymphatic system impairment in multiple sclerosis: relation with brain damage and disability. Brain 2022;145:2785-2795.ArticlePubMedPDF
- 29. Zhang X, Wang Y, Jiao B, et al. Glymphatic system impairment in Alzheimer’s disease: associations with perivascular space volume and cognitive function. Eur Radiol 2024;34:1314-1323.ArticlePubMedPDF
- 30. Zhang X, Wang W, Bai X, et al. Increased glymphatic system activity in migraine chronification by diffusion tensor image analysis along the perivascular space. J Headache Pain 2023;24:147.ArticlePubMedPMCPDF
- 31. Yuan Z, Li W, Tang H, et al. Enlarged perivascular spaces in patients with migraine: a case-control study based on 3T MRI. Ann Clin Transl Neurol 2023;10:1160-1169.ArticlePubMedPMC
- 32. Wu CH, Chang FC, Wang YF, et al. Impaired glymphatic and meningeal lymphatic functions in patients with chronic migraine. Ann Neurol 2024;95:583-595.ArticlePubMed
- 33. Wardlaw JM, Smith EE, Biessels GJ, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol 2013;12:822-838.ArticlePubMedPMC
- 34. Zhang W, Cheng Z, Fu F, Zhan Z. Prevalence and clinical characteristics of white matter hyperintensities in Migraine: a meta-analysis. Neuroimage Clin 2023;37:103312.ArticlePubMedPMC
- 35. Ornello R, Bruno F, Frattale I, et al. White matter hyperintensities in migraine are not mediated by a dysfunction of the glymphatic system: a diffusion tensor imaging magnetic resonance imaging study. Headache 2023;63:1128-1134.ArticlePubMed
- 36. Zhang Y, Li Y, He L. Correlation between migraine and cerebral small vessel disease: a case-control study. Eur J Pain 2024;28:551-564.ArticlePubMed
- 37. Lee DA, Lee HJ, Park KM. Normal glymphatic system function in patients with migraine: a pilot study. Headache 2022;62:718-725.ArticlePubMedPDF
- 38. Husøy AK, Indergaard MK, Honningsvåg LM, et al. Perivascular spaces and headache: a population-based imaging study (HUNT-MRI). Cephalalgia 2016;36:232-239.ArticlePubMedPDF
- 39. Jeon CW, Lim GY, Moon JU. Dedicated neuroimaging analysis in children with primary headaches: prevalence of lesions and a comparison between patients with and without migraines. BMC Med Imaging 2023;23:152.ArticlePubMedPMCPDF
- 40. Lewis DW, Dorbad D. The utility of neuroimaging in the evaluation of children with migraine or chronic daily headache who have normal neurological examinations. Headache 2000;40:629-632.ArticlePubMed
- 41. Schick S, Gahleitner A, Wöber-Bingöl C, et al. Virchow-Robin spaces in childhood migraine. Neuroradiology 1999;41:283-287.ArticlePubMedPDF
- 42. Vittorini MG, Sahin A, Trojan A, et al. The glymphatic system in migraine and other headaches. J Headache Pain 2024;25:34.ArticlePubMedPMCPDF
- 43. Toriello M, González-Quintanilla V, Pérez-Pereda S, Fontanillas N, Pascual J. The potential role of the glymphatic system in headache disorders. Pain Med 2021;22:3098-3100.ArticlePubMedPDF
- 44. Liu X, Wu G, Tang N, et al. Glymphatic drainage blocking aggravates brain edema, neuroinflammation via modulating TNF-α, IL-10, and AQP4 after intracerebral hemorrhage in rats. Front Cell Neurosci 2021;15:784154.ArticlePubMedPMC
- 45. Kepp O, Galluzzi L, Zitvogel L, Kroemer G. Pyroptosis: a cell death modality of its kind? Eur J Immunol 2010;40:627-630.ArticlePubMed
- 46. Rainville JR, Hodes GE. Inflaming sex differences in mood disorders. Neuropsychopharmacology 2019;44:184-199.ArticlePubMedPMCPDF
- 47. Gu S, Li Y, Jiang Y, Huang JH, Wang F. Glymphatic dysfunction induced oxidative stress and neuro-inflammation in major depression disorders. Antioxidants (Basel) 2022;11:2296.ArticlePubMedPMC
- 48. Thuraiaiyah J, Erritzøe-Jervild M, Al-Khazali HM, Schytz HW, Younis S. The role of cytokines in migraine: a systematic review. Cephalalgia 2022;42:1565-1588.ArticlePubMedPDF
- 49. Messlinger K. The big CGRP flood: sources, sinks and signalling sites in the trigeminovascular system. J Headache Pain 2018;19:22.ArticlePubMedPMCPDF
- 50. Lohela TJ, Lilius TO, Nedergaard M. The glymphatic system: implications for drugs for central nervous system diseases. Nat Rev Drug Discov 2022;21:763-779.ArticlePubMedPDF
- 51. Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science 2013;342:373-377.ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Chronic Migraine Is Associated With Region-Specific High-Grade Enlarged Perivascular Spaces: Retrospective Matched Case-Control Study
Jae Wook Cho, Gha-Hyun Lee, Jiyoung Kim
Journal of Clinical Neurology.2026; 22(1): 113. CrossRef - Diffusion Tensor Imaging-Based Glymphatic Dysfunction Assessments in Migraine Syndromes: Mechanisms and Diagnostic Implications
Emily Lai, Joshua Estin, Jiahao Zhou, Roger Sheffmaker, Manisha Koneru
Biomedicines.2025; 13(12): 2981. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
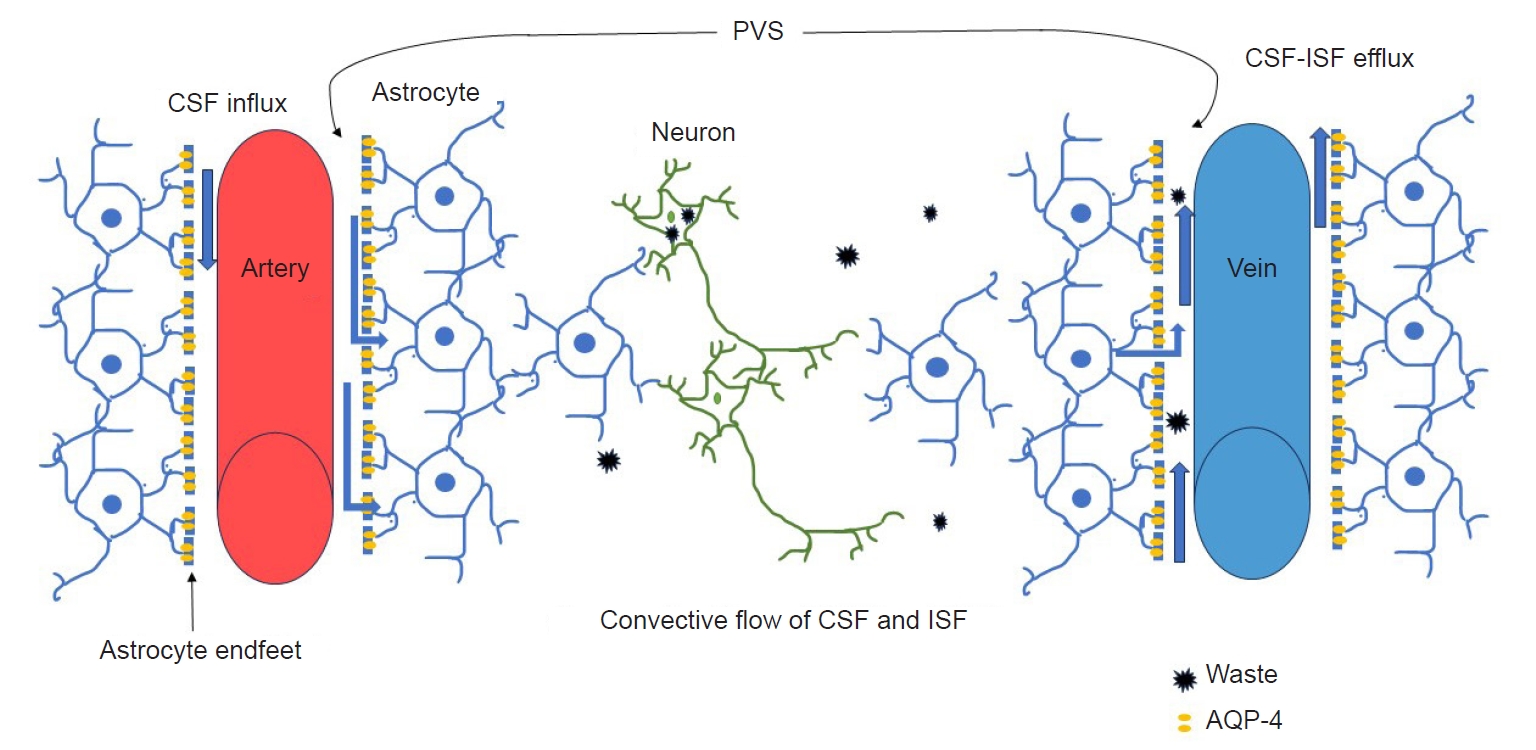
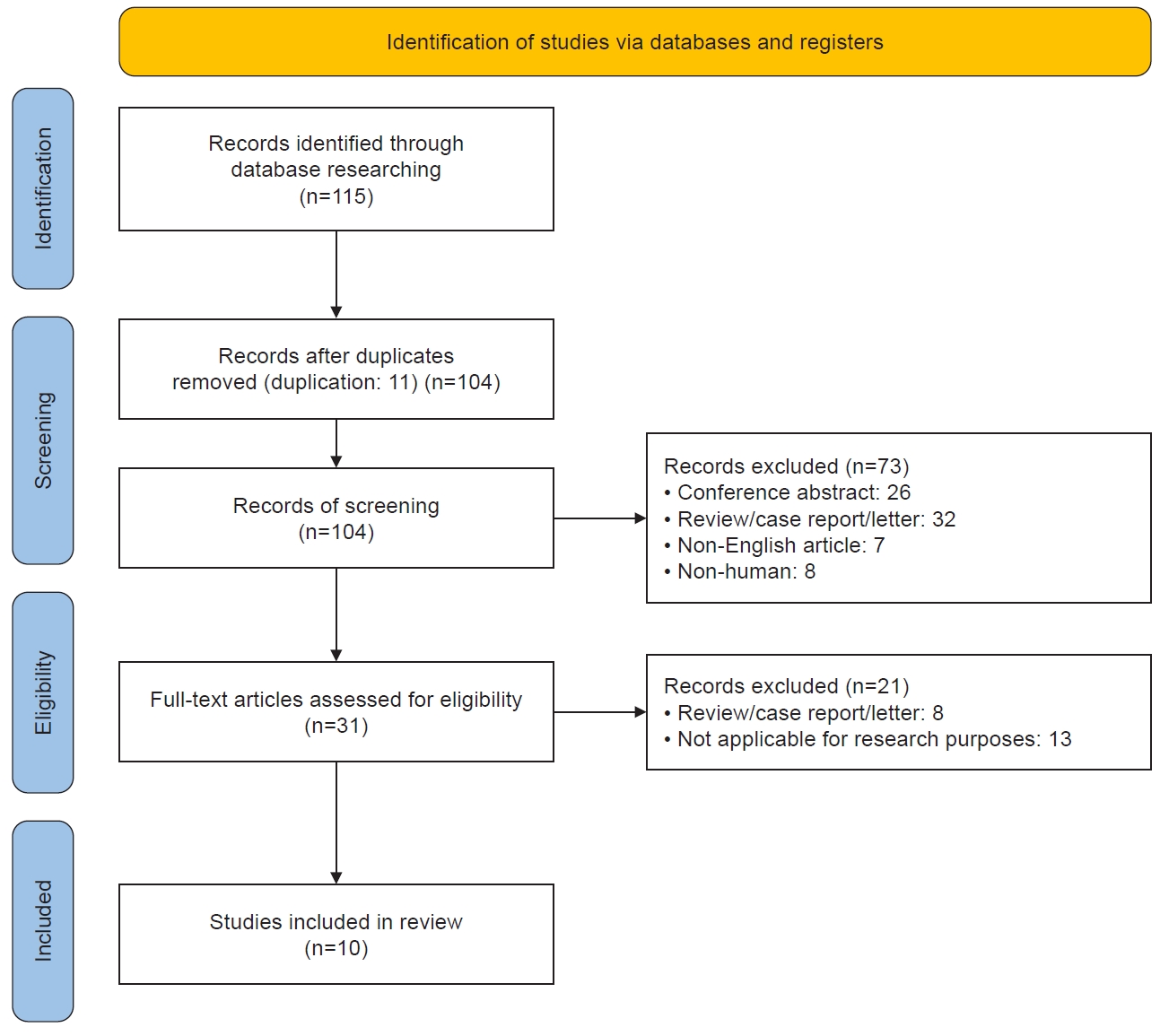
Figure 1.
Figure 2.
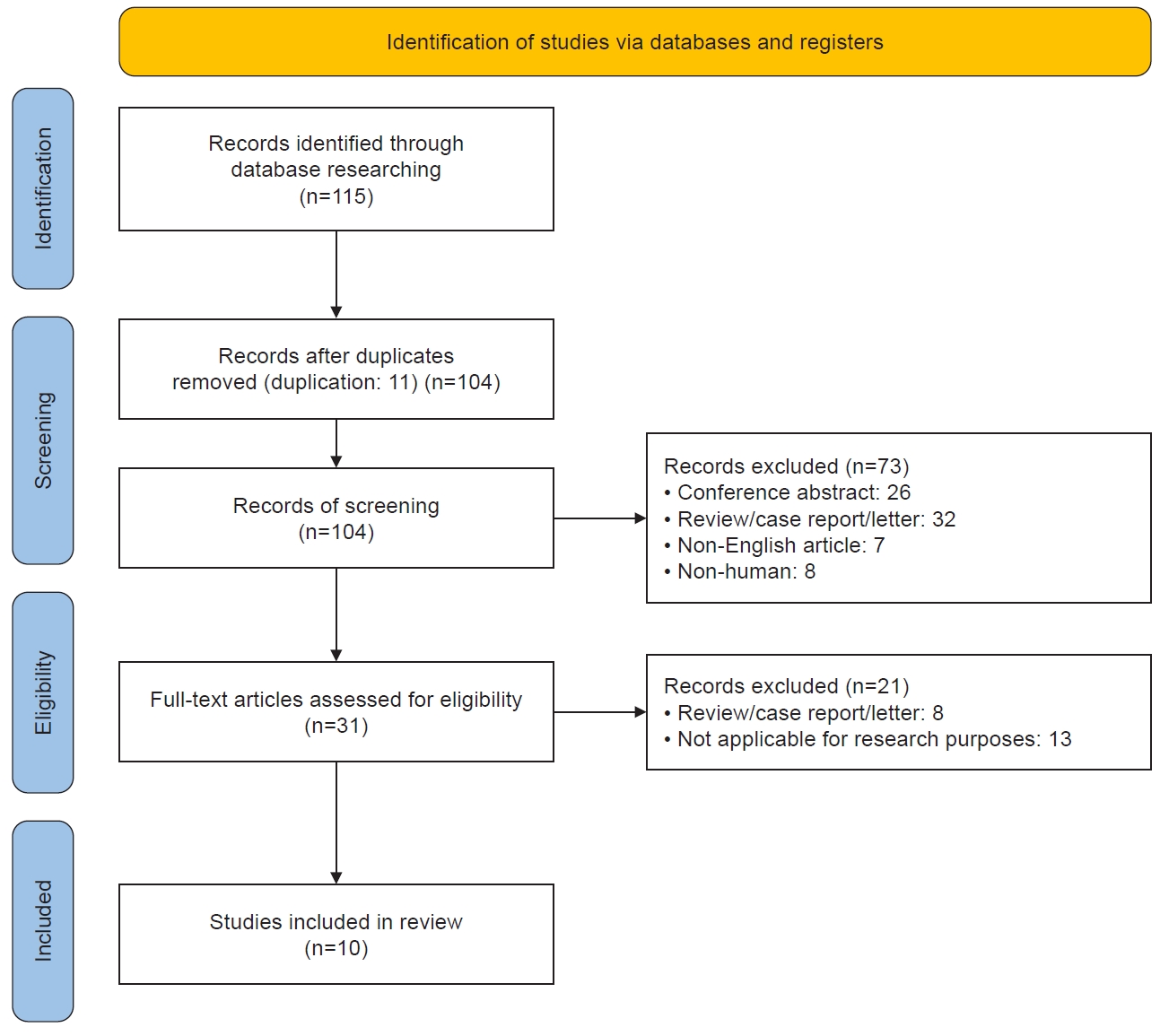
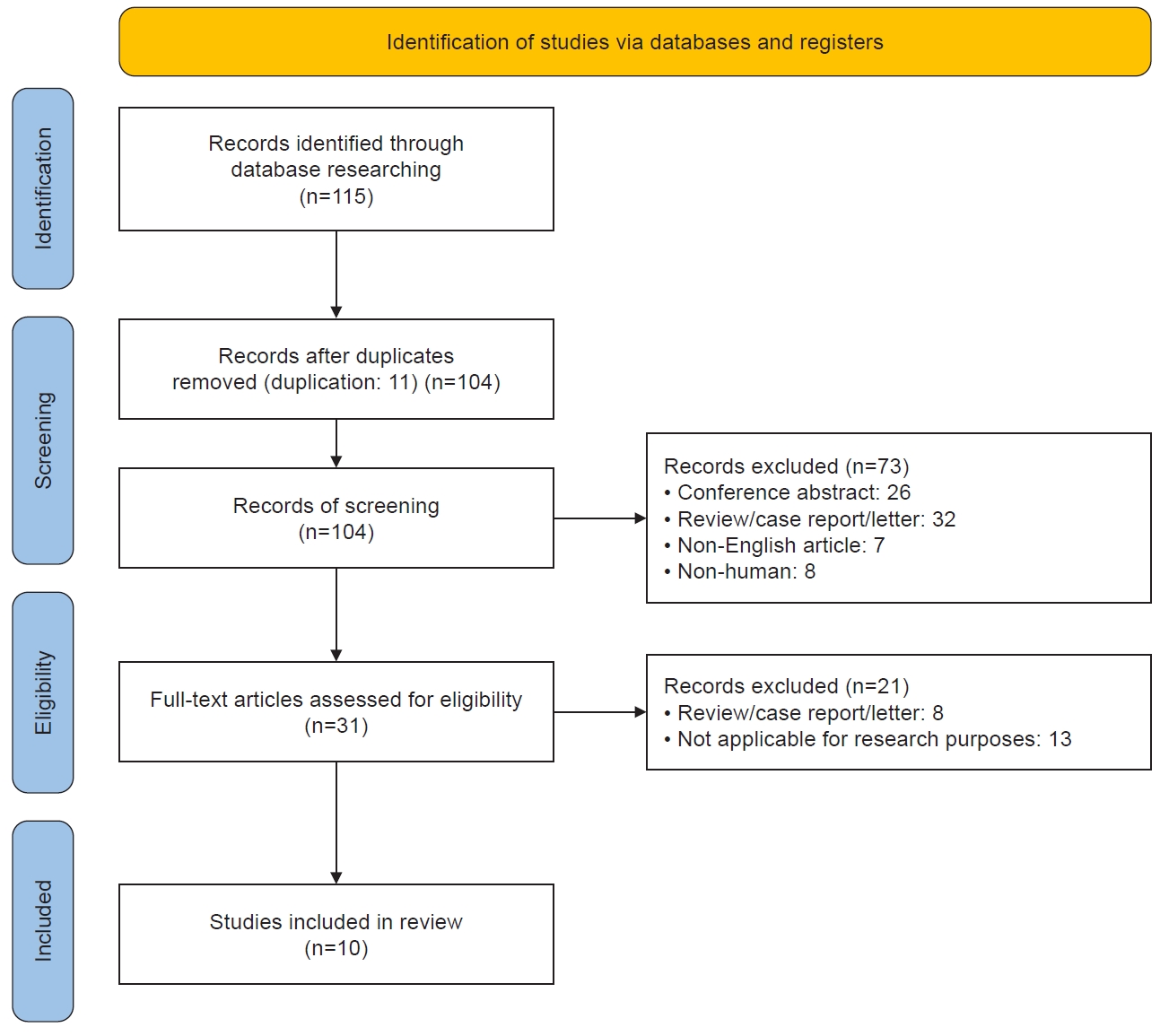
| Inclusion criteria | Exclusion criteria |
|---|---|
| English studies | Reviews, meta-analyses, case reports, letter and/or conference proceedings, conference abstracts |
| Migraine must be diagnosed according to the ICHD-3 or earlier guidelines published by the International Headache Society | Non-English |
| Study outcomes must be related to the glymphatic system and migraine | Non-human |
| Study | Location | Study design | Participants (n) | Diagnostic criteria | Age (yr)* | Study including only children† | Female/male ratio | GS assessment tool | Main outcome |
|---|---|---|---|---|---|---|---|---|---|
| Zhang et al. (2024) [36] | China | Case-control study | Migraine (48) | ICHD-3 | Migraine: 31.0 (25.5–34.0) | NA | 1.7:1 | Visual inspection of MRI | Migraine with aura was negatively correlated with the number of VRS in basal ganglia. |
| TTH (32) | TTH: 32.5 (27.5–35.5) | Visual rating scale (Potter et al. [22], (2015); https://www.ed.ac.uk/files/imports/fileManager/epvs-rating-scale-user-guide.Pdf) | Education level and migraine frequency were correlated with the number of VRS. | ||||||
| HC (49) | HC: 32.0 (24.0–37.0) | ||||||||
| Zhang et al. (2023) [30] | China | Cross-sectional study | EM (32) | ICHD-3 | EM: 34.8±15.4 | NA | 1.9:1 | DTI-ALPS index | CM had a higher DTI-ALPS index in the right hemisphere than EM and HC. |
| CM (24) | CM: 34.8±16.8 | ||||||||
| HC (41) | HC: 36.0±10.9 | ||||||||
| Jeon et al. (2023) [39]‡ | Korea | Cross-sectional study | Migraine (46) | ICHD-3 or earlier | UN | Only children | UN | Visual inspection of MRI | Dilatated PVS was the most common finding in the migraine and non-migraine headache groups. |
| Non-migraine (60) | |||||||||
| Ornello et al. (2023) [35] | Italy | Cross-sectional study | EM and CM (147) | ICHD-3 | EM and CM: 45 (36–50) | NA | 4.4:1 | DTI-ALPS index | White matter hyperintensity was not associated with an impairment in the glymphatic system in patients with migraine. |
| Yuan et al. (2023) [31] | China | Case-control study | EM (59) | ICHD-3 | EM: 39 (32–43) | NA | 2.4:1 | Visual inspection of MRI | Migraineurs had a significantly higher prevalence of high-grade enlarged PVS in centrum semiovale and midbrain than HC. |
| CM (115) | CM: 42 (33–48) | Visual rating scale (Potter et al. [22] (2015); https://www.ed.ac.uk/files/imports/fileManager/epvs-rating-scale-user-guide.Pdf) | |||||||
| HC (57) | HC: 41 (30–47) | ||||||||
| Wu et al. (2024) [32] | Taiwan | Cross-sectional study | EM (73) | ICHD-3 | EM: 37.4±10.2 | NA | 3.7:1 | DTI-ALPS index | The DTI-ALPS index was lower in CM than in EM and HC. |
| CM (39) | CM: 36.2±11.5 | Dynamic contrast-enhanced MRI for meningeal lymphatic vessels. | |||||||
| HC (63) | HC: 39.7±8.0 | ||||||||
| Lee et al. (2022) [37] | Korea | Cross-sectional study | MA (20) | ICHD-3 | MA: 36.0±12.9 | NA | 3.9:1 | DTI-ALPS index | The DTI-ALPS index did not differ between migraine patients and HC. |
| MO (72) | MO: 38.4±11.3 | ||||||||
| HC (80) | HC: 37.8±11.7 | ||||||||
| Husøy et al. (2016) [38] | Norway | Cross sectional and longitudinal study | Total (1,006) | ICHD-2 | Total range: 50–66 | NA | UN | Visual inspection and counting of visible PVS | In the cross-sectional analysis, fewer PVS were observed in migraine without aura. However, in the longitudinal analysis, there was no significant association between the number of PVS and headache, including migraine. |
| Lewis et al. (2000) [40] | United States | Cross-sectional study | Total (302) | ICHD-1-R§ | Total range: 6–18 | Only children | UN | Visual inspection of CT and MRI | Among 42 migraine patients undergoing CT scans, dilated VRS were observed in one subject. |
| Migraine (107) | |||||||||
| Schick et al. (1999) [41] | Austria | Case-control study | Migraine (31 children) | ICHD-1 | Range: 3–14 (children) | Only children (in group of migraine, TTH and headache-free children) | 1.1 (in group of migraine and TTH) | Visual inspection of MRI | The prevalence of VRS in childhood migraine was higher than in those with TTH, headache-free children, or adults with migraine. |
| TTH (27 children) | 22–55 (adults) | ||||||||
| Controls (30 headache-free children) | |||||||||
| Controls (30 migraine adult) |
ICHD, International Classification of Headache Disorders.
GS, glymphatic system; TTH, tension-type headache; HC, healthy controls; ICHD, International Classification of Headache Disorders; NA, not applicable; MRI, magnetic resonance imaging; VRS, Virchow-Robin spaces; EM, episodic migraine; CM, chronic migraine; DTI-ALPS, diffusion tensor image analysis along the perivascular spaces; PVS, perivascular spaces; MA, migraine with aura; MO, migraine without aura; UN, uncertain; CT, computed tomography. *Age is reported as median (interquartile range), mean±standard deviation, or range only. †A child is 18 years of age or younger. ‡The subgroup analysis results are exclusively associated with the glymphatic system, making the demographic characteristics of the participants unclear. §ICHD-1-R was proposed as a modification based on the ICHD-1.
Table 1.
Table 2.
TOP
 KHS
KHS