Abstract
-
Purpose
- Although strict unilaterality is a characteristic of cluster headache (CH), side shift of attacks has been reported. We aimed to assess the prevalence and patterns of side shifts, as well as their correlations with clinical characteristics and treatment response in CH patients.
-
Methods
- We prospectively recruited and followed up CH patients at a university hospital. Patients with two or more lifetime CH bouts were interviewed about their side shift history using a structured questionnaire. The demographics and disease characteristics were collected at baseline, and the treatment response at 2- to 4-week follow-up examinations was compared between patients with versus without side shifts.
-
Results
- Out of 124 CH patients, 26 (21.0%) experienced side shifts. Sixteen (61.5%) experienced shifts between bouts, 13 (50.0%) within a bout, and four (15.4%) within an attack, with none (0%) reporting bilateral pain during an attack. Among patients who experienced shifts between bouts, six (37.5%) reported a single shift during the entire disease course, while 10 (62.5%) reported multiple shifts between bouts. The demographics, characteristics, and treatment response did not significantly differ according to the history of side shift.
-
Conclusion
- In our study, the prevalence and pattern of side shifts were comparable to the results from earlier studies. The presence of side shifts did not show significant association with a specific clinical profile and their incidence did not impact the treatment response. These findings suggest that side-shifting CH is not a distinct entity or migraine variant, but rather within the spectrum of CH.
-
Keywords: Cluster headache, Headache, Trigeminal autonomic cephalalgias
INTRODUCTION
Cluster headache (CH) is a type of headache characterized by unilateral orbital, supraorbital, or temporal pain accompanied by distinct autonomic symptoms such as tearing, conjunctival injection, ptosis, miosis, swelling of the eyelid, rhinorrhea, nasal congestion, and forehead sweating on the same side as the headache.1 The strict unilaterality, often referred to as side-locked headache, is a characteristic feature of CHs. Some patients may experience a phenomenon known as side shift, where the location of the headache shifts from one side to the other.
When considering why such side shift occurs in CHs, one might speculate whether changes in hypothalamic activation are occurring, and if so, whether they involve hormonal or structural alterations. According to current research, activation of the trigeminovascular system alone, which innervates cranial nerve vessels through divisions of the trigeminal nerve, cannot fully explain the characteristic circadian periodicity of CHs. Therefore, the hypothalamus, acting as the brain's biological clock, is believed to function as the generator of CHs. Neuroimaging findings support this hypothesis.2-4 For instance, positron emission tomography scans taken during a patient's acute pain state have shown activation in the ipsilateral inferior hypothalamic grey matter.4 However, while alterations in hypothalamic activity on one side are documented, the reasons behind the phenomenon of side shift in CHs remain unclear. Understanding the factors that induce changes in the hypothalamus or other pain-matrix networks is important for comprehending the pathogenesis of CHs. Therefore, investigating the clinical correlates of side shift could provide further insights. Moreover, if side shift is linked to alterations in hypothalamic activity, a core mechanism of CHs, it could impact treatment outcomes and disease progression. Hence, it is reasonable to assume that the presence or absence of side shift may lead to variations in treatment efficacy and disease course. Consequently, this study aimed to explore whether there are disparities in the prevalence and patterns of side shift among patients and to investigate any differences in demographics, clinical characteristics, and treatment response based on the presence or absence of side shift.
MATERIALS AND METHODS
1. Ethics approval and consent to participate
Written informed consent forms were obtained from all patients included and this study was approved by the Institutional Review Board (IRB) of Samsung Medical Center (IRB #2018-10-029).
2. Study design and participants
Patients with CH who experienced two or more lifetime CH bouts were prospectively recruited at Samsung Medical Center and followed up from October 2016 to December 2021. The diagnosis of CH was made by neurologists with headache expertise according to International Classification of Headache Disorders-3 (ICHD-3) criteria.5
3. Prevalence and patterns of side shifts
Side shift was defined as unilateral headache occurring in CH where pain had switched to the other side, whenever it happens. When patients were asked on which side the pain had occurred, they were also asked to answer if the pain had ever switched sides and if the pain had ever occurred bilaterally, as well. This question was asked for the current and all the previous bouts. If the patient answered that the side of pain had switched during the disease course, they were further asked whether the pain remained on one side after the switch or if it shifted multiple times, whether the pain was bilateral, whether shifts occurred within a bout, and if shifts only occur in different bouts. They were allowed to answer ‘yes’ to more than one answer. With the answers to the above questions, side shift patterns that the patients experienced were classified into three categories: shifts occurring between bouts, within a bout, or within an attack, where one can experience more than one side shift pattern. If side shift occurred between bouts, patients were asked whether the shift occurred only once or more than once, occurring multiple times. In patients who experienced shifts during an attack, whether bilateral pain occurred was also examined.
4. Data collection and assessment
Data were collected on patients’ demographics, including age, sex, body mass index, and smoking history, disease characteristics at baseline, characteristics of the current bout, and treatment response to acute and preventive medications. The data collected on patients’ disease characteristics included onset age, disease duration (years), average cluster and remission periods (in weeks and in months, respectively), the total number of bouts, diurnal and seasonal rhythmicity, comorbid migraine, and the recurrence pattern (regular vs. irregular). Data regarding the current bout were also collected, including the frequency, intensity, and duration of attacks and the duration of the current bout. Data on treatment responses were followed up after 2–4 weeks. Treatment response was defined as ≥50% reduction in headache frequency for preventive medications and ≥50% reduction in pain intensity for acute medication.
5. Statistical analysis
Categorical data are presented as numbers (percentages) and continuous variables are presented as median (interquartile range). Prevalence of side shifts were determined. In patients with side shifts, the percentage of those who experienced shifts between bouts, within a bout, and within an attack were analyzed, and in those who experienced between-bout shifts, side shift pattern during a bout was also analyzed (strictly unilateral vs. alternating in a single bout). Because not all patients have responded on the treatment response, the number of patients who have answered to have had treatment response and the percentage of patients with treatment response among those who have responded were presented as number (%). Demographic data, baseline clinical characteristics of attacks and bouts, and treatment response of preventive and acute medications were compared between CH patients with and without side shifts using Student t-test or Fisher’s exact test. Treatment response was also compared between patients with and without side shifts. All statistical analyses were done using SPSS version 27 software (IBM Corp.).
RESULTS
1. Demographics and disease characteristics
Out of 124 patients enrolled in the study, 106 (85.5%) were male and 18 (14.5%) were female, resulting in a male to female ratio of 5.9:1, reflecting the male predominance of CH. Only one patient had chronic CH.
No significant difference was observed between CH patients with and without side shifts regarding age, sex, body mass index, smoking habits, onset age, years after CH onset, average cluster period, average remission period, total number of bouts, the presence of diurnal or seasonal rhythmicity, comorbidity of migraine, and the recurrence pattern, whether it was regular or irregular (Table 1). With regards to the characteristics of the current bout, statistically significant difference between attack frequency, intensity, and duration, and duration of cluster period was not observed (p=0.193, 0.696, 0.842, and 0.675, respectively).
Out of 98 patients without side shift, 65 (66.3%) and 33 patients (33.7%) answered to have pain on the right and the left side, respectively, in the current bout. Among 26 patients who answered to have had experienced side shifts, the pain was on the right side in 10 patients (38.5%), on the left side in seven (26.9%), and on both sides in nine (34.6%) during the current bout.
2. Side shift: prevalence and patterns
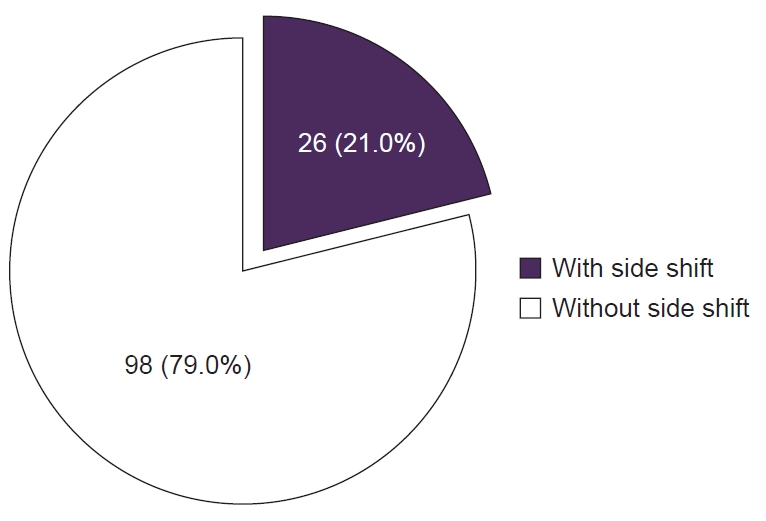
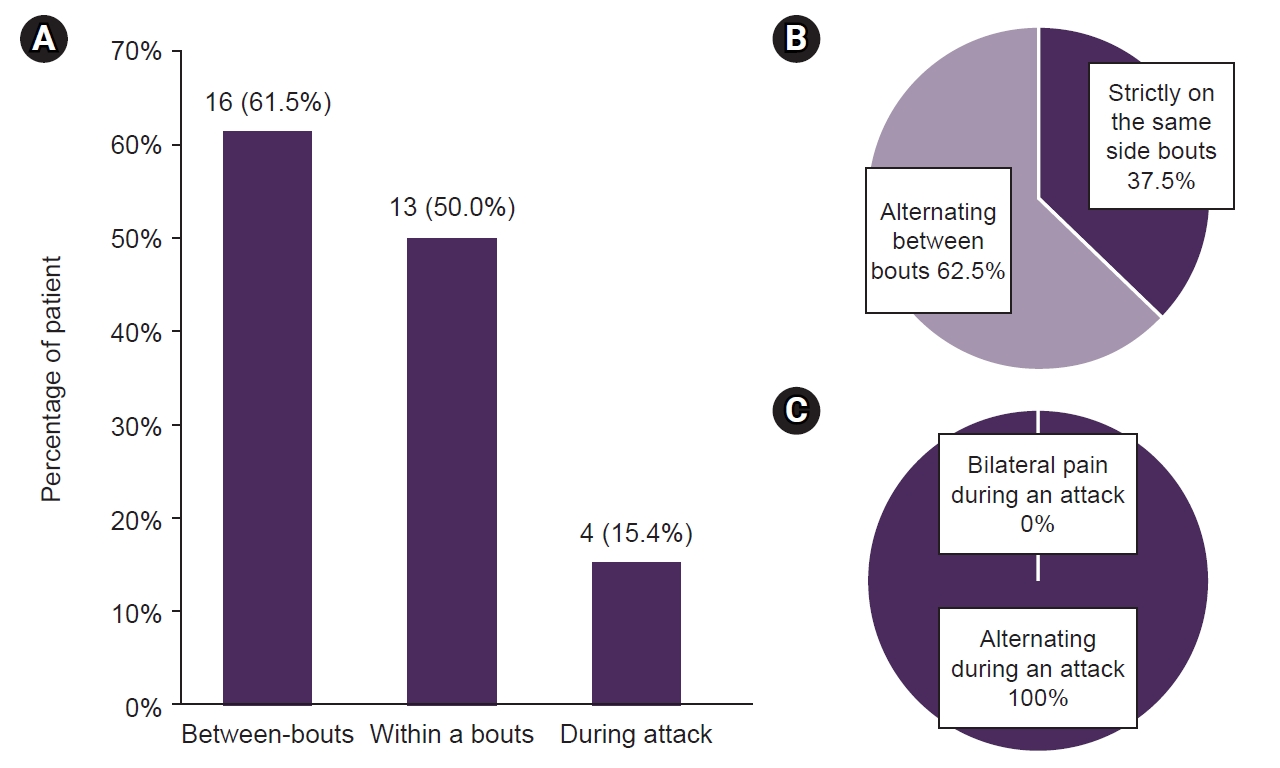
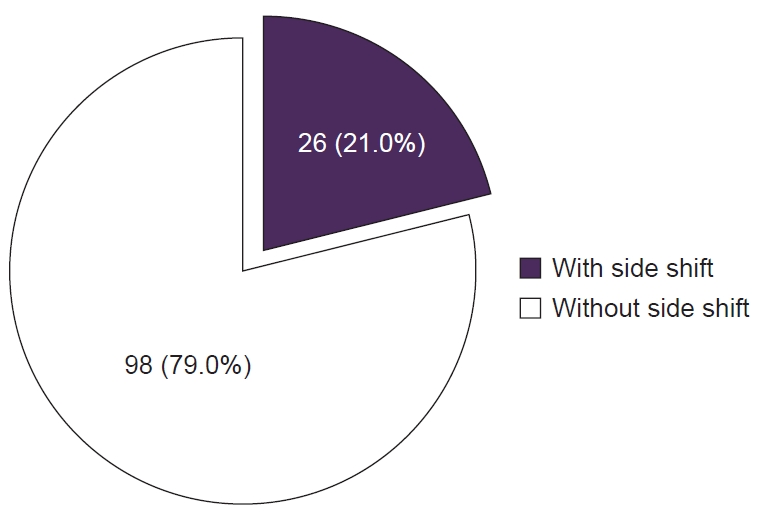
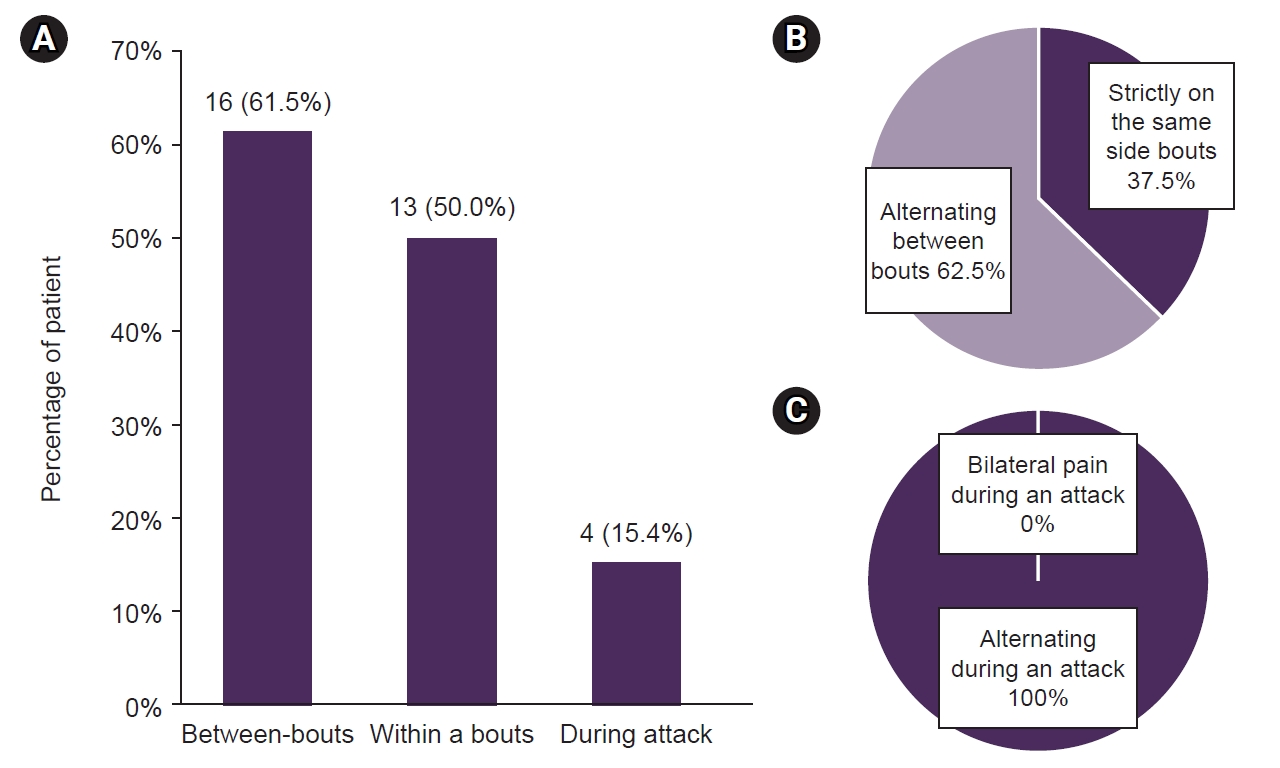
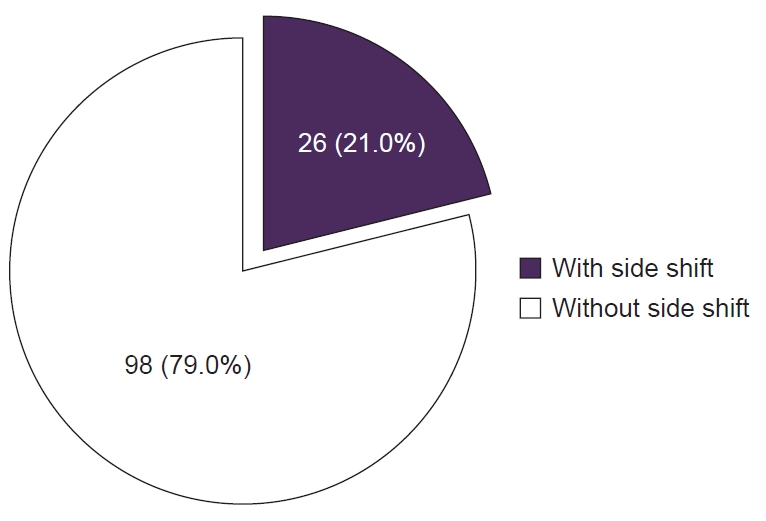
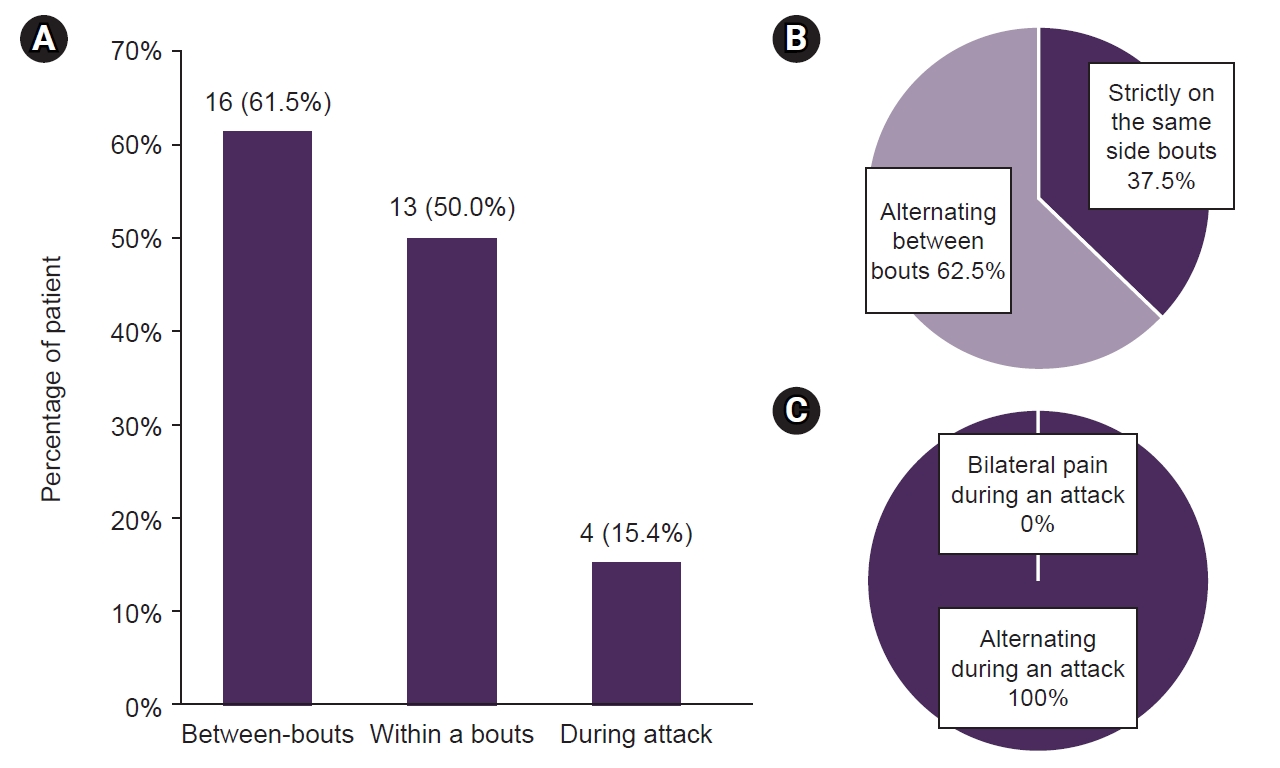
A total of 26 patients (21.0%) have experienced side shifts (Figure 1). Regarding the side shift patterns among 26 patients who have experienced side shifts, 16 (61.5%) have experienced between-bouts shifts, 13 patients (50.0%) have experienced shifts within a bout, and four (15.4%) during an attack (Figure 2A). Patients who had experienced between-bouts side shifts were asked on the unilaterality of the pain, and six (37.5%) responded that the pain strictly remained on the same side once a side shift occurred and 10 (62.5%) responded that the side of the pain alternated between bouts (Figure 2B). None of the patients responded that they had experienced bilateral pain during an attack (Figure 2).
3. Treatment response: with side shift vs. without side shift
No significant difference was observed in the treatment response of preventive medications (oral prednisone, verapamil, and lithium) between patients with and without side shift (p=0.399, 0.154, and 0.173, respectively) (Table 2). In the comparison of treatment responses of acute medications (nonsteroidal anti-inflammatory drugs and triptan), no significant difference was found between those with and without side shift (p>0.999 and =0.649, respectively) (Table 2).
DISCUSSION
The major findings of this study are as follows. 1) About 1/5 of CH patients had experienced at least one type of side shift, 2) Side shift occurred between bouts, within a bout, or during an attack. 3) Side shifts were not associated with distinct clinical profile or treatment response.
While CH typically exhibits a strictly unilateral pain pattern, studies suggest that side shifts occur in 14.0%–23.5% of CH cases, consistent with our findings.6-11 For instance, a German study found that 33 out of 209 patients (15.8%) experienced side shifts during their CH disease.6 A Nordic multicenter study from 2009 reported that 55 out of 383 CH patients (14.0%) had encountered pain side shifts.7 Additionally, a prospective study in Greece by Vikelis and Rapoport11 indicated that 12.6% of 302 CH patients had encountered some form of side shift. In a Danish cross-sectional cohort study involving 540 CH patients investigating factors associated with the transition between chronic and episodic phenotypes, 127 patients (23.5%) reported shifting sides of attacks.10 These various international studies collectively challenge the notion of the strict unilateral nature of pain in CH patients.
We found that side shifts occur between bouts, during bouts, and during attacks. Between-bout shift was the most common type, then within a bout, and then during an attack. This aligns with findings from Bahra et al.,6 who reported that 8.6% of CH patients experienced side shifts between or within bouts and 1.9% during an attack. Rozen and Fishman8 found that 31.0% of CH patients had side shifts between bouts or attacks within a bout, and 8.0% reported side shifts during an attack. In a study by Vikelis and Rapoport,11 side shifts occurred most frequently between bouts, followed by within bouts and within attacks (9.0%, 3.0%, 1.7%, respectively), consistent with our study results. Søborg et al.10 reported side shifts in 23.5% of patients, with 8.7% occurring between bouts, 8.1% during a bout, and 5.2% during attacks in episodic CH patients, which resembles the results observed in our study. A study in China has shown the prevalence of side shift to be 30.8%,12 and as our current study is the first report on the prevalence and side shift patterns in Koreans, side shift patterns seem to be similar in different ethnicities, although further prospective studies in many more diverse populations will be needed. However, a cohort study in Germany by Schürks et al.9 showed some diversity, with 18.7% of 246 patients indicating a change in the side of pain, and 2.8% reporting bilateral pain during an attack, in contrast to our study where none reported experiencing bilateral pain during an attack. Thus, further studies on side shift patterns in various populations may contribute to predicting disease course and treatment responses according to side shift patterns in different ethnicities.
The occurrence of side shifts was not found to be linked to a distinct clinical profile. Previous studies focused on the association between side shift and disease subtype.7,10 Meyer et al.7 reported that the prevalence of pain side shifts did not exhibit a significant difference between individuals with chronic and episodic CH (13.0% vs. 15.0%). Søborg et al.10 found that the prevalence of side shifts at any time point was highest in secondary chronic CH patients compared to primary episodic patients (33.3% vs. 19.1%). Although our study included a very small proportion of patients with chronic CH, a longitudinal data might be required in the future to validate previous study findings on the prognosis of CH patients with side shift. Our study is the first comprehensive examination of clinical profiles comparing patients with and without side shift. Moreover, side shifts were not associated with treatment response to acute or preventive medications. Taken together, our finding indicates that CH with side shift is not a clinically distinct entity, and this may suggest that side shift does not reflect a different pathophysiology.
The strength of this study is that the patients included in the study were diagnosed with CH according to the ICHD-3 criteria and were interviewed with detailed questionnaires made by an experienced headache specialist. Also, not many studies analyzed many aspects of CH in correlation with the presence of side shift, including treatment response. This study analyzed the preventive and acute treatment response of CH patients, including the relationship between treatment response and the presence of side shifts, which to our knowledge is the first time and has not been evaluated in previous studies.
This study has several limitations. Because the patients were asked to respond to questionnaires about all the past bouts and attacks, the possibility of recall bias exists. It would have been helpful if data on onset of the first side shift was also collected and analyzed. As chronic CH is known to be rare in Asian populations compared to Europe and the United States,13 chronic CH is also rare in Korea,14 and comprehensive comparison between episodic and chronic CH was not done because only one patient had chronic CH in this study. Only <1% of patients had chronic CH in our study, which is even lower than 5.3% reported in previous Korean data.14 This might be attributed to differences in study design and setting. More data on the chronic CH will be needed to test if there is a difference in side shift patterns between episodic and chronic CH. Also, among patients who had answered that they have experienced side shifts, not all patients answered the pattern of the side shift, so the prevalence of each side shift pattern may not be complete.
Understanding this side shifting phenomenon to be a spectrum of CH is important because this may lead to misdiagnosis of CH as migraine and lead to delayed diagnosis and appropriate treatment.
AVAILABILITY OF DATA AND MATERIAL
The data presented in this study are available upon reasonable request from the corresponding author.
AUTHOR CONTRIBUTIONS
Conceptualization: MSY, JPK; Data curation: JPK, MJL; Formal analysis: all authors; Funding acquisition: MJL; Investigation: MSY, MJL; Methodology: JPK, MJL; Project administration: MSY, MJL; Resources: MJL; Software: JPK, MJL; Supervision: MJL; Validation: MJL; Visualization: MSY; Writing–original draft: MSY; Writing–review & editing: all authors.
CONFLICT OF INTEREST
Mi Ji Lee has been the editor of Headache and Pain Research since 2023 and was not involved in the review process. And, she has received personal or institutional honoraria for participation in clinical trials, speaker fees, or as a consultant from Abbvie, Biohaven, Eli Lilly, Lundbeck, Novartis, Otsuka, Sanofi-Aventis, SK Pharm, Teva, Yuhan Company, and YuYu Pharma.
Other authors have no other conflicts of interest to declare.
FUNDING STATEMENT
This study was supported by the New Faculty Startup Fund from Seoul National University, the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIP; No. 2020R1A2B5B01001826 to MJL), and Yuhan company (for the data management). The funders had no role in study design, data analysis, and drafting.
ACKNOWLEDGMENTS
Not applicable.
Figure 1.Prevalence of side shifts in patients with cluster headache (CH). Out of 124 CH patients, 26 (21.0%) experienced side shifts.
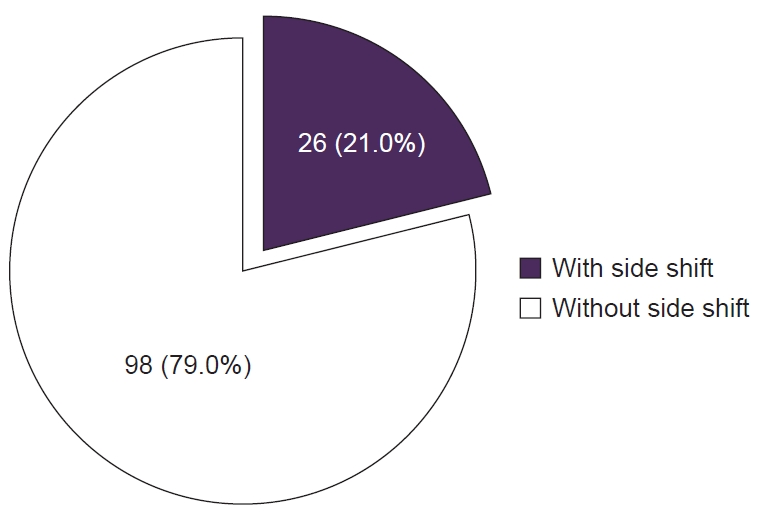
Figure 2.Patterns of side shift. Among 26 patients who experienced side shifts, (A) 16 patients (61.5%) experienced shifts between bouts, 13 (50.0%) experienced shifts within a bout, and four (15.4%) experienced shifts during an attack. (B) In patients who experienced between-bout side shifts, six (37.5%) stated that the pain remained strictly on the same side once a between-bout side shift occurred, while 10 (62.5%) answered that the pain side changed between bouts. (C) None of the patients who experienced side shifts during an attack stated that they had experienced bilateral pain during an attack.
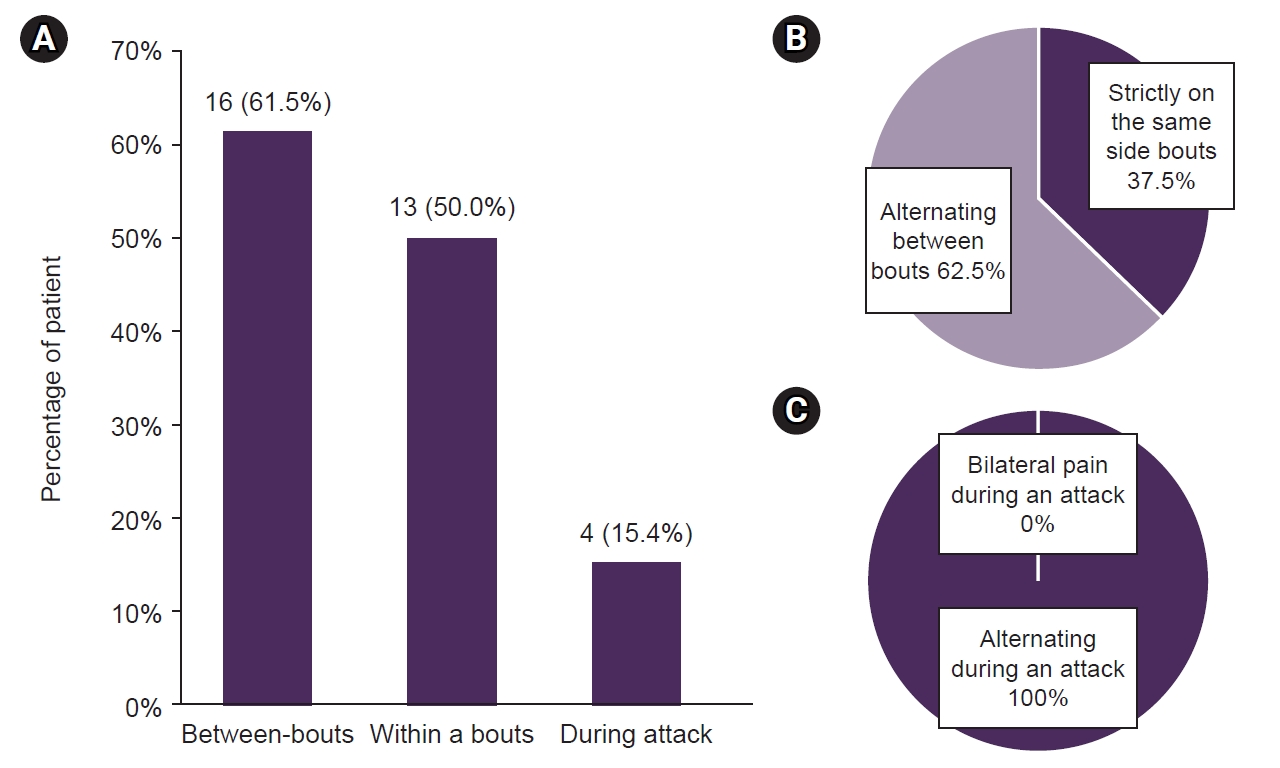
Table 1.Demographics and clinical characteristics of participants
|
Side shift |
p-value |
|
Absent (n=98) |
Present (n=26) |
|
Demographics |
|
|
|
|
Age (yr) |
35.5 (27.5–43.0) |
35.0 (27.0–43.5) |
0.927 |
|
Female |
12 (15.0) |
6 (28.6) |
0.198 |
|
Body mass index (kg/m2) |
24.3 (22.0–26.8) |
23.5 (20.1–26.2) |
0.225 |
|
Smoking |
|
|
0.188 |
|
Current smoker |
31 (38.8) |
8 (38.1) |
|
|
Ex-smoker |
21 (26.2) |
2 (9.5) |
|
Never |
28 (35.0) |
11 (52.4) |
|
Clinical characteristics |
|
|
|
|
Onset age (yr) |
23.50 (17.00–32.75) |
21.00 (17.00–29.00) |
0.574 |
|
Years after CH onset |
9 (5–14) |
9 (5–14) |
0.508 |
|
Average cluster period (wk) |
4.0 (3.0–7.0) |
4.0 (2.5–7.0) |
0.505 |
|
Average remission period (mo) |
11 (9–12) |
11 (10–23) |
0.217 |
|
Total number of bouts |
7.0 (4.0–12.0) |
9.0 (4.0–13.5) |
0.889 |
|
Diurnal rhythmicity |
37 (46.8) |
12 (57.1) |
0.401 |
|
Seasonal rhythmicity |
39 (50.0) |
12 (57.1) |
0.561 |
|
Migraine |
7 (8.8) |
3 (14.3) |
0.430 |
|
Regular recurrence pattern |
55 (68.8) |
12 (60.0) |
0.457 |
|
Irregular recurrence pattern |
25 (31.3) |
8 (40.0) |
0.457 |
|
Attack frequency per day (times) |
1.00 (1.00–2.00) |
1.50 (1.00–3.25) |
0.193 |
|
Attack intensity, NRS |
9.5 (8.5–10.0) |
9.5 (9.0–10.0) |
0.696 |
|
Attack duration (min) |
90.0 (60.0–150.0) |
90.0 (42.5–150.0) |
0.842 |
|
Duration of current cluster bout (day) |
38.5 (22.8–60.3) |
48.0 (25.0–74.0) |
0.675 |
Table 2.Comparison of acute and preventive medication treatment responses
|
Side shift |
Total (n=124) |
p-value |
|
Absent (n=98) |
Present (n=26) |
|
Preventive medication |
|
|
|
|
|
Oral prednisone |
34 (97.1) |
9 (90.0) |
43 (95.6) |
0.399 |
|
Verapamil |
38 (86.4) |
9 (69.2) |
47 (82.5) |
0.154 |
|
Lithium |
23 (88.5) |
3 (60.0) |
26 (83.9) |
0.173 |
|
Acute medication |
|
|
|
|
|
NSAIDs |
35 (85.4) |
7 (87.5) |
42 (85.7) |
>0.999 |
|
Triptan |
39 (81.3) |
6 (75.0) |
45 (80.4) |
0.649 |
REFERENCES
- 1. Kim M, Yu JK, Kim YH. Update on cluster headaches: from genetic to novel therapeutic approaches. Headache Pain Res 2024;25:42-53.ArticlePDF
- 2. Láinez MJ, Guillamón E. Cluster headache and other TACs: pathophysiology and neurostimulation options. Headach 2017;57:327-335.ArticlePDF
- 3. Leone M, Bussone G. A review of hormonal findings in cluster headache. Evidence for hypothalamic involvement. Cephalalgia 1993;13:309-317.ArticlePubMedPDF
- 4. May A, Bahra A, Büchel C, Frackowiak RS, Goadsby PJ. Hypothalamic activation in cluster headache attacks. Lancet 1998;352:275-278.ArticlePubMed
- 5. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018;38:1-211.ArticlePDF
- 6. Bahra A, May A, Goadsby PJ. Cluster headache: a prospective clinical study with diagnostic implications. Neurology 2002;58:354-361.ArticlePubMed
- 7. Meyer EL, Laurell K, Artto V, et al. Lateralization in cluster headache: a Nordic multicenter study. J Headache Pain 2009;10:259-263.ArticlePubMedPMCPDF
- 8. Rozen TD, Fishman RS. Cluster headache in the United States of America: demographics, clinical characteristics, triggers, suicidality, and personal burden. Headache 2012;52:99-113.ArticlePubMed
- 9. Schürks M, Kurth T, de Jesus J, Jonjic M, Rosskopf D, Diener HC. Cluster headache: clinical presentation, lifestyle features, and medical treatment. Headache 2006;46:1246-1254.ArticlePubMed
- 10. Søborg MK, Petersen AS, Lund N, Wandall-Holm MF, Jensen RH, Barloese M. Transition of cluster headache phenotype: an interview-based study. Cephalalgia 2023;43:3331024221128287.ArticlePubMed
- 11. Vikelis M, Rapoport AM. Cluster headache in Greece: an observational clinical and demographic study of 302 patients. J Headache Pain 2016;17:88.ArticlePubMedPMCPDF
- 12. Xie Q, Huang Q, Wang J, Li N, Tan G, Zhou J. Clinical features of cluster headache: an outpatient clinic study from China. Pain Med 2013;14:802-807.ArticlePubMed
- 13. Peng KP, Takizawa T, Lee MJ. Cluster headache in Asian populations: similarities, disparities, and a narrative review of the mechanisms of the chronic subtype. Cephalalgia 2020;40:1104-1112.ArticlePubMedPMCPDF
- 14. Lee MJ, Park JW, Chu MK, et al. Treatment pattern and response for cluster headache in Korea: a prospective multicenter observation study. Cephalalgia 2023;43:3331024231159627.ArticlePubMedPDF
Citations
Citations to this article as recorded by

- Pain Lateralization in Cluster Headache and Associated Clinical Factors
Soohyun Cho, Mi Ji Lee, Min Kyung Chu, Jeong Wook Park, Heui-Soo Moon, Pil-Wook Chung, Jong-Hee Sohn, Byung-Su Kim, Daeyoung Kim, Kyungmi Oh, Byung-Kun Kim, Soo-Jin Cho
Journal of Clinical Neurology.2025; 21(3): 220. CrossRef
 , Jun Pyo Kim2
, Jun Pyo Kim2 , Mi Ji Lee3
, Mi Ji Lee3

 PubReader
PubReader ePub Link
ePub Link Cite this Article
Cite this Article
 KHS
KHS