Articles
- Page Path
- HOME > Headache Pain Res > Volume 25(2); 2024 > Article
-
Original Article
Subjective Cognitive Decline Patterns in Patients with Migraine, with or without Depression, versus Non-depressed Older Adults -
Sun Hwa Lee
 , Soo-Jin Cho
, Soo-Jin Cho
-
Headache and Pain Research 2024;25(2):103-110.
DOI: https://doi.org/10.62087/hpr.2024.0022
Published online: October 24, 2024
Department of Neurology, Hallym University Dongtan Sacred Heart Hospital, Hwaseong, Republic of Korea
- Correspondence: Sun Hwa Lee, M.A. Department of Neurology, Hallym University Dongtan Sacred Heart Hospital, 7 Keunjaebong-gil, Hwaseong 18450, Republic of Korea Tel: +82-31-8086-2310, Fax: +82-31-8086-2317, E-mail: sunhwa520@hotmail.com
© 2024 The Korean Headache Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 4,809 Views
- 49 Download
Abstract
-
Purpose
- Cognitive decline is a common complaint in young patients with migraine, especially those with depression. Independent of psychiatric factors such as depression, subjective cognitive decline (SCD) is associated with an elevated risk of progression to dementia. This study aimed to investigate patterns of subjective cognitive complaints between migraineurs with or without depression and non-depressed older adults.
-
Methods
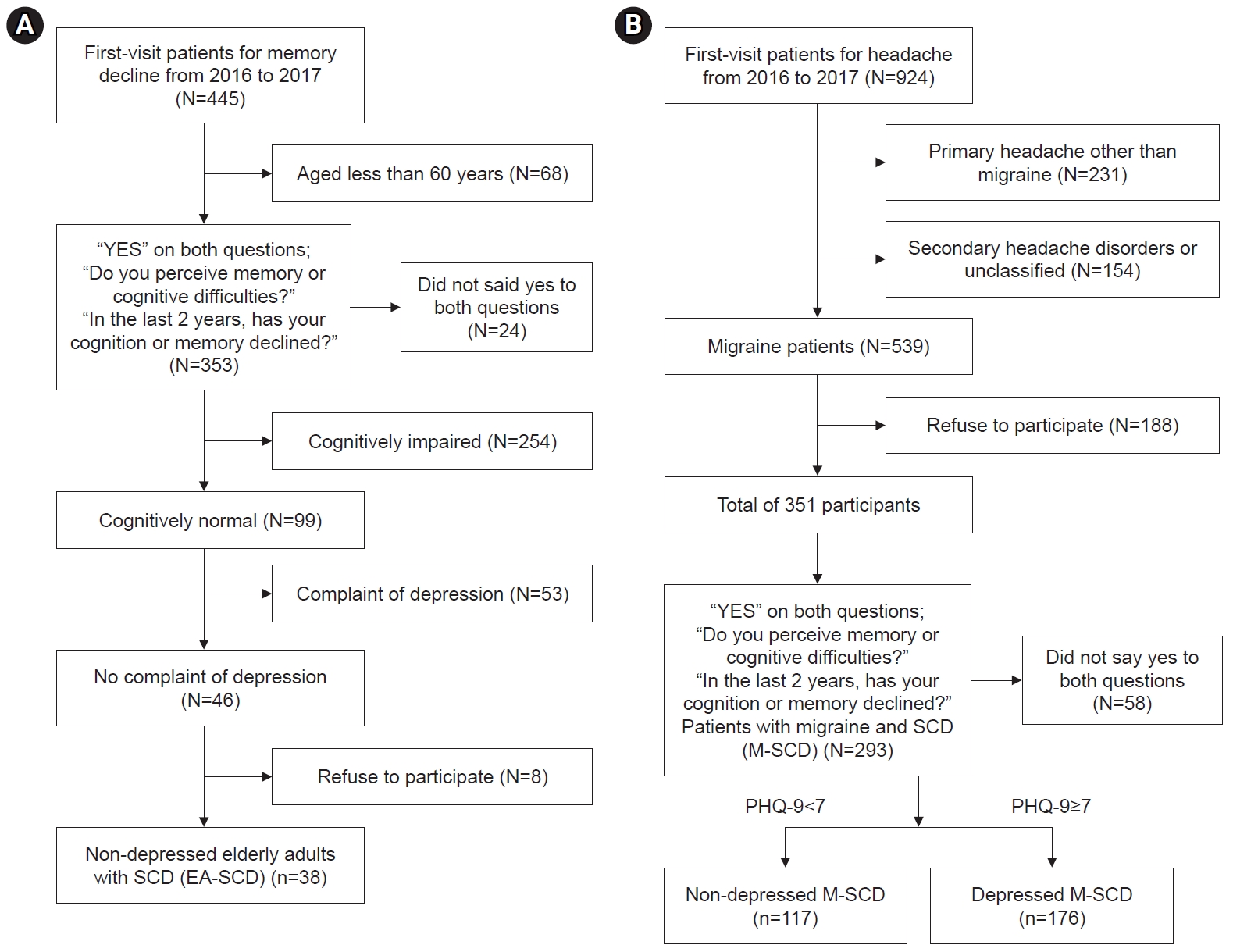
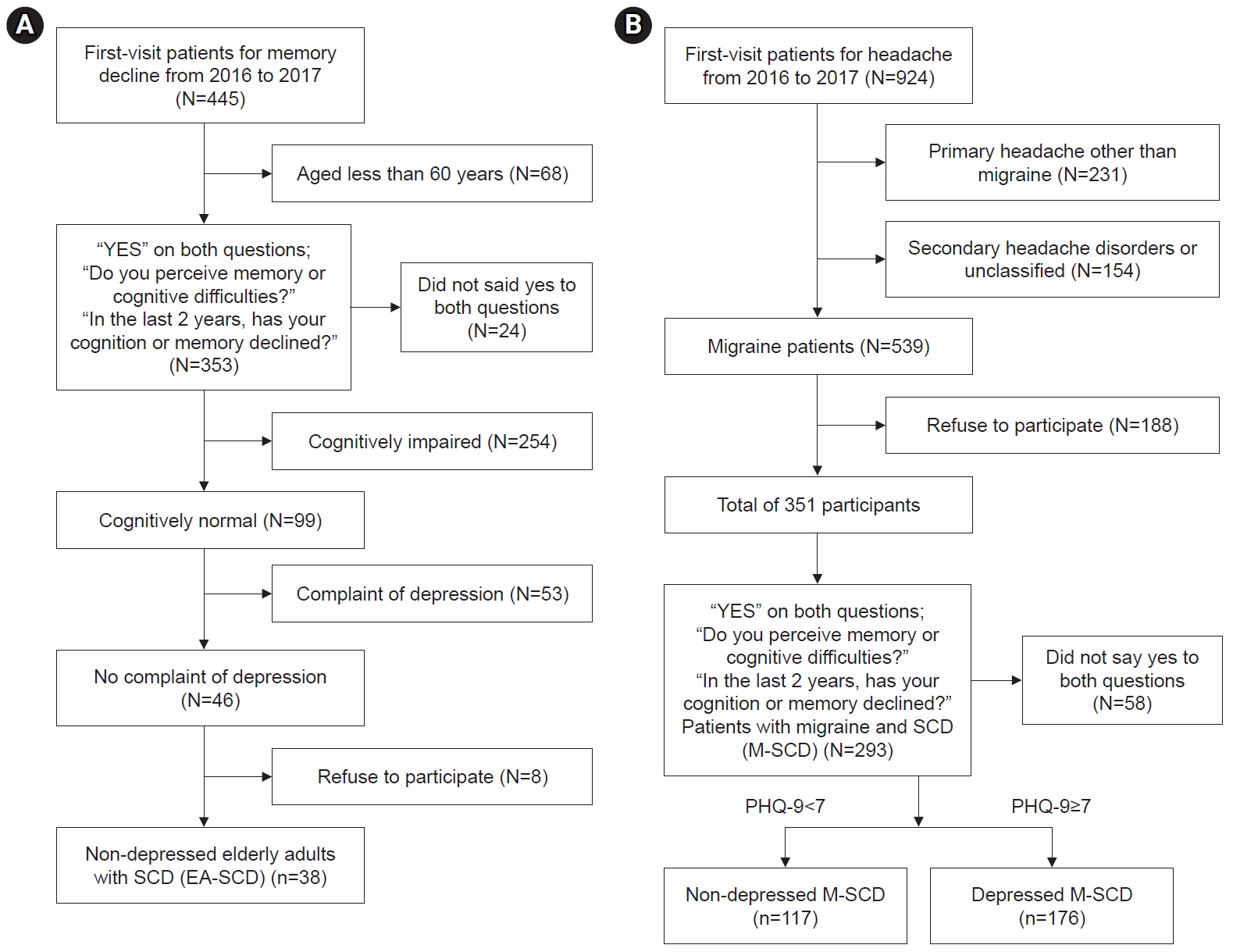
- This retrospective study included 331 outpatients with SCD (293 from a headache clinic and 38 from a memory clinic). SCD was diagnosed as “yes” based on two questions about SCD. The Mini Mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA) were used to assess cognitive function. The SCD Questionnaire (SCD-Q) with three subdomains was analyzed to compare SCD between groups.
-
Results
- Among patients with SCD, significant differences in duration of education were found among the groups—specifically, migraineurs with depression (12.39 years) had longer education than non-depressed older adults (10.50 years) and shorter education than migraineurs without depression (14.28 years). The total MMSE and MoCA scores did not differ between migraineurs with and without depression. Regarding SCD-Q scores, migraineurs with depression showed higher scores overall and in all cognitive domains than migraineurs without depression, with no significant difference compared to non-depressed older adults.
-
Conclusion
- Although the depressed migraineurs with SCD were younger and more educated than the non-depressed older adults with SCD, both groups reported similarly high levels of SCD. Higher levels of surveillance for cognitive decline are warranted for migraineurs with depression who have SCD.
INTRODUCTION
MATERIALS AND METHODS
RESULTS
DISCUSSION
AVAILABILITY OF DATA AND MATERIAL
Anonymized data supporting the findings presented in the current study will be shared upon reasonable request from a qualified investigator.
AUTHOR CONTRIBUTIONS
Conceptualization: SHL, SJC; Data curation: SHL; Investigation: SHL; Writing–original draft: SHL; Writing–review & editing: SHL, SJC.
All authors have read and agreed to the published version of the manuscript.
CONFLICT OF INTEREST
Soo-Jin Cho is the Editor-in-Chief of the Headache and Pain Research since 2023 and was not involved in the review process of this article. All authors have no other conflicts of interest to declare.
FUNDING STATEMENT
Not applicable.
ACKNOWLEDGMENTS
Not applicable.
Values are presented as mean±standard deviation or number only.
Group A, non-depressed elderly adults with subjective cognitive decline; Group B, non-depressed patients with migraine and subjective cognitive decline (non-depressed M-SCD); Group C, depressed patients with migraine and subjective cognitive decline (depressed-M-SCD); ns, not significant; MMSE, Mini Mental State Examination; MoCA, Montreal Cognitive Assessment.
Values are presented as mean±standard deviation.
SCD-Q, subjective cognitive decline Questionnaire; Group A, non-depressed elderly adults with subjective cognitive decline (EA-SCD); Group B, non-depressed patients with migraine and subjective cognitive decline (non-depressed M-SCD); Group C, depressed patients with migraine and subjective cognitive decline (depressed-M-SCD).
- 1. World Health Organization (WHO). Global action plan on the public health response to dementia 2017–2025 [Internet] WHO; 2017 [cited 2024 July 17]. Available from: https://www.who.int/publications/i/item/global-action-plan-on-the-public-health-response-to-dementia-2017---2025
- 2. Haney MS, Pálovics R, Munson CN, et al. APOE4/4 is linked to damaging lipid droplets in Alzheimer’s disease microglia. Nature 2024;628:154-161.ArticlePubMedPMCPDF
- 3. Jessen F, Amariglio RE, Buckley RF, et al. The characterisation of subjective cognitive decline. Lancet Neurol 2020;19:271-278.ArticlePubMedPMC
- 4. Meiberth D, Scheef L, Wolfsgruber S, et al. Cortical thinning in individuals with subjective memory impairment. J Alzheimers Dis 2015;45:139-146.ArticlePubMed
- 5. Rabin LA, Smart CM, Crane PK, et al. Subjective cognitive decline in older adults: an overview of self-report measures used across 19 international research studies. J Alzheimers Dis 2015;48 Suppl 1:S63-S86.ArticlePubMed
- 6. Amariglio RE, Becker JA, Carmasin J, et al. Subjective cognitive complaints and amyloid burden in cognitively normal older individuals. Neuropsychologia 2012;50:2880-2886.ArticlePubMedPMC
- 7. Snitz BE, Lopez OL, McDade E, et al. Amyloid-β imaging in older adults presenting to a memory clinic with subjective cognitive decline: a pilot study. J Alzheimers Dis 2015;48 Suppl 1:S151-S159.ArticlePubMed
- 8. Ali JI, Smart CM, Gawryluk JR. Subjective cognitive decline and APOE ɛ4: a systematic review. J Alzheimers Dis 2018;65:303-320.ArticlePubMed
- 9. Desai R, Whitfield T, Said G, et al. Affective symptoms and risk of progression to mild cognitive impairment or dementia in subjective cognitive decline: a systematic review and meta-analysis. Ageing Res Rev 2021;71:101419.ArticlePubMed
- 10. Tolner EA, Chen SP, Eikermann-Haerter K. Current understanding of cortical structure and function in migraine. Cephalalgia 2019;39:1683-1699.ArticlePubMedPMCPDF
- 11. Kim S, Park JW. Migraines in women: a focus on reproductive events and hormonal milestones. Headache Pain Res 2024;25:3-15.ArticlePDF
- 12. Kim JH, Kwon YS, Lee SH, Sohn JH. Associations of migraine and tension-type headache with glaucoma. Headache Pain Res 2024;25:54-62.ArticlePDF
- 13. Lee SH, Kang Y, Cho SJ. Subjective cognitive decline in patients with migraine and its relationship with depression, anxiety, and sleep quality. J Headache Pain 2017;18:77.ArticlePubMedPMCPDF
- 14. Gil-Gouveia R, Martins IP. Cognition and cognitive impairment in migraine. Curr Pain Headache Rep 2019;23:84.ArticlePubMedPDF
- 15. Gu L, Wang Y, Shu H. Association between migraine and cognitive impairment. J Headache Pain 2022;23:88.ArticlePubMedPMCPDF
- 16. Begasse de Dhaem O, Robbins MS. Cognitive impairment in primary and secondary headache disorders. Curr Pain Headache Rep 2022;26:391-404.ArticlePubMedPMCPDF
- 17. Rami L, Mollica MA, García-Sanchez C, et al. The subjective cognitive decline questionnaire (SCD-Q): a validation study. J Alzheimers Dis 2014;41:453-466.ArticlePubMed
- 18. Seo JG, Park SP. Validation of the Patient Health Questionnaire-9 (PHQ-9) and PHQ-2 in patients with migraine. J Headache Pain 2015;16:65.ArticlePubMedPMCPDF
- 19. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018;38:1-211.ArticlePDF
- 20. Kang Y, Jahng S, Na D. Seoul Neuropsychological Screening Battery (SNSB), 2nd ed. Human Brain. Research & Consulting Co.. 2012.
- 21. Cho MJ, Bae JN, Suh GH, et al. Validation of geriatric depression scale, Korean version (GDS) in the assessment of DSM-III-R major depression. J Korean Neuropsychiatr Assoc 1999;38:48-63.
- 22. Kang Y, Na DL, Hahn S. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc 1997;15:300-308.
- 23. Kang Y, Park J, Yu KH, Lee BC. A reliability, validity, and normative study of the Korean-Montreal Cognitive Assessment (K-MoCA) as an instrument for screening of vascular cognitive impairment (VCI). Korean J Clin Psychol 2009;28:549-562.Article
- 24. Lee SH, Kim MH, Sohn JH, Cho SJ. Mindfulness-based cognitive therapy for patients with migraine. Korean J Headache 2019;20:37-41.
- 25. Braganza DL, Fitzpatrick LE, Nguyen ML, Crowe SF. Interictal Cognitive deficits in migraine sufferers: a meta-analysis. Neuropsychol Rev 2022;32:736-757.ArticlePubMedPDF
- 26. Gerstein MT, Wirth RJ, Uzumcu AA, et al. Patient-reported experiences with migraine-related cognitive symptoms: results of the MiCOAS qualitative study. Headache 2023;63:441-454.ArticlePubMedPDF
REFERENCES
Figure & Data
References
Citations

 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
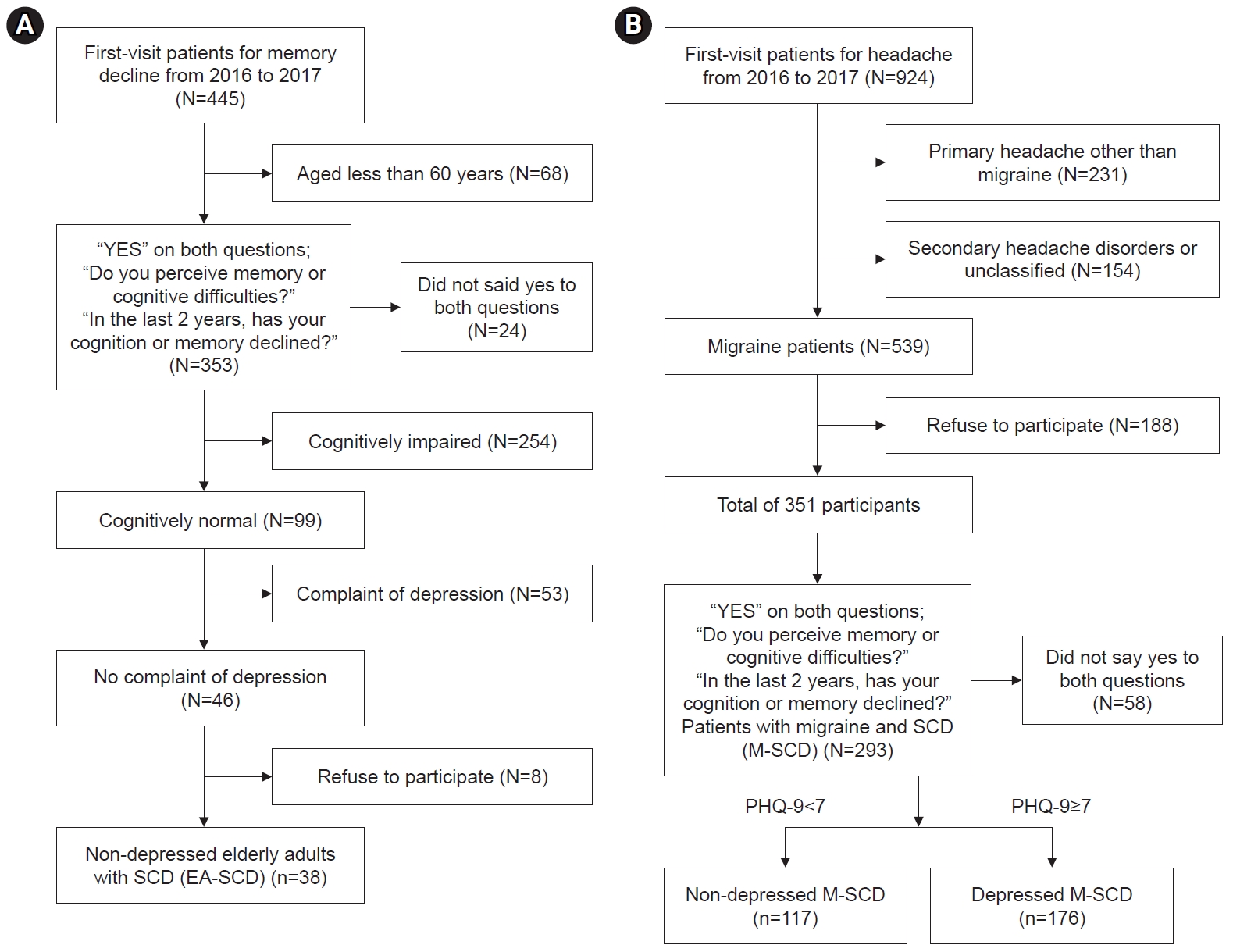
Figure 1.
| Cognitive domain | No. | SCD-Q items |
|---|---|---|
| Memory | 1 | I find it harder to learn new telephone numbers. |
| 2 | I find it harder to find personal possessions (keys, telephone, utensils, etc.). | |
| 3 | I find it harder to describe the plots of films. | |
| 4 | I find it harder to remember doctor’s appointments. | |
| 5 | I find it harder to follow the plot of a book. | |
| 6 | I’m worse at recalling the details of a book. | |
| 7 | I find it harder to remember the result of a recent sporting event. | |
| 8 | I find it harder to remember sums of money (payments or debts). | |
| 9 | I find it harder to remember the details of a conversation. | |
| 10 | I find it harder to remember things without using strategies (lists, diary, etc.). | |
| 11 | I find it harder to remember the details of recent news. | |
| Language | 12 | I find it harder to remember famous people’s names. |
| 13 | I find it harder to remember the names of people I’ve met recently. | |
| 14 | I find it harder to remember street and city names. | |
| 15 | I’m worse at finding the word I want to use in a conversation. | |
| 16 | I find it harder to understand things the first time someone says them. | |
| 17 | I find it harder to remember the names of places I’ve visited recently. | |
| Executive | 18 | I find it harder to concentrate on what I am doing. |
| 19 | I’m worse at planning things that aren’t part of my daily routine (travel, excursions, etc.). | |
| 20 | I find it harder to use electronic devices. | |
| 21 | I find it harder to start new or different things. | |
| 22 | I find it harder to start conversations. | |
| 23 | I find it harder to do mental arithmetic. | |
| 24 | I find it harder to do more than one thing at once without getting agitated. |
| Group A (n=38) | Group B (n=117) | Group C (n=176) | p-value | Post-hoc | |
|---|---|---|---|---|---|
| Age (yr) | 66.03±7.44 | 41.23±10.03 | 42.67±12.13 | <0.001 | A>B=C |
| Education (yr) | 10.50±4.37 | 14.28±2.83 | 12.39±3.57 | <0.001 | A<C<B |
| Sex ratio (female:male) | 28:10 | 92:25 | 133:43 | 0.761 | ns |
| MMSE total score | 27.97±1.60 | 28.92±1.25 | 28.34±2.23 | 0.020 | A<B, A=C, B=C |
| MoCA total score | 24.08±1.71 | 27.39±2.05 | 26.48±3.32 | <0.001 | A<B=C |
| SCD-Q | Group A (n=38) | Group B (n=117) | Group C (n=176) | p-value | Post-hoc |
|---|---|---|---|---|---|
| Total score | 10.11±5.55 | 6.79±3.80 | 10.39±5.39 | <0.001 | A=C>B |
| Memory domain score | 4.50±3.04 | 3.08±2.18 | 4.81±2.92 | <0.001 | A=C>B |
| Language domain score | 3.24±1.57 | 2.14±1.45 | 2.74±1.69 | <0.001 | A=C>B |
| Executive domain score | 2.37±1.97 | 1.58±1.30 | 2.85±1.92 | <0.001 | A=C>B |
Values are presented as mean±standard deviation or number only. Group A, non-depressed elderly adults with subjective cognitive decline; Group B, non-depressed patients with migraine and subjective cognitive decline (non-depressed M-SCD); Group C, depressed patients with migraine and subjective cognitive decline (depressed-M-SCD); ns, not significant; MMSE, Mini Mental State Examination; MoCA, Montreal Cognitive Assessment.
Values are presented as mean±standard deviation. SCD-Q, subjective cognitive decline Questionnaire; Group A, non-depressed elderly adults with subjective cognitive decline (EA-SCD); Group B, non-depressed patients with migraine and subjective cognitive decline (non-depressed M-SCD); Group C, depressed patients with migraine and subjective cognitive decline (depressed-M-SCD).
Table 1.
Table 2.
Table 3.
TOP
 KHS
KHS