Articles
- Page Path
- HOME > Headache Pain Res > Volume 26(1); 2025 > Article
-
Review Article
Update on Tension-type Headache -
Hye Jeong Lee1
 , Soo-Jin Cho2
, Soo-Jin Cho2 , Jong-Geun Seo3
, Jong-Geun Seo3 , Henrik Winther Schytz4
, Henrik Winther Schytz4
-
Headache and Pain Research 2025;26(1):38-47.
DOI: https://doi.org/10.62087/hpr.2024.0025
Published online: December 30, 2024
1Department of Neurology, Chung-Ang University Gwangmyeong Hospital, Gwangmyeong, Republic of Korea
2Department of Neurology, Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Republic of Korea
3Department of Neurology, School of Medicine, Kyungpook National University, Daegu, Republic of Korea
4Headache Diagnostic Laboratory, Danish Headache Center and Department of Neurology, Rigshospitalet Glostrup, Faculty of Health Sciences, University of Copenhagen, Glostrup, Denmark
- Correspondence: Hye Jeong Lee, M.D. Department of Neurology, Chung-Ang University Gwangmyeong Hospital, 110 Deokan-ro, Gwangmyeong 14353, Republic of Korea, Tel: +82-2-1811-7800, Fax: +82-2-2610-6624, E-mail: hjlee@cauhs.or.kr
© 2025 The Korean Headache Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 38,108 Views
- 835 Download
- 6 Crossref
Abstract
- Tension-type headache (TTH) is the most common type of headache, characterized by mild to moderate intensity, bilateral, with a pressing or tightening (non-pulsating) quality. Migraine and TTH can occur in the same person, and their risk factors and treatments can overlap. However, TTH receives less attention than migraine. Furthermore, despite the expanding market for migraine treatments targeting calcitonin gene-related peptide (CGRP) mechanisms, the lack of evidence regarding mechanisms related to CGRP-related mechanisms in TTH continues to be neglected. There remains a need to develop effective preventive treatments for chronic TTH, which imposes a very high burden of disease. From this perspective, this review aims to provide the latest evidence on TTH.
INTRODUCTION
EPIDEMIOLOGY
CLINICAL PRESENTATION
DIAGNOSIS
PATHOPHYSIOLOGY
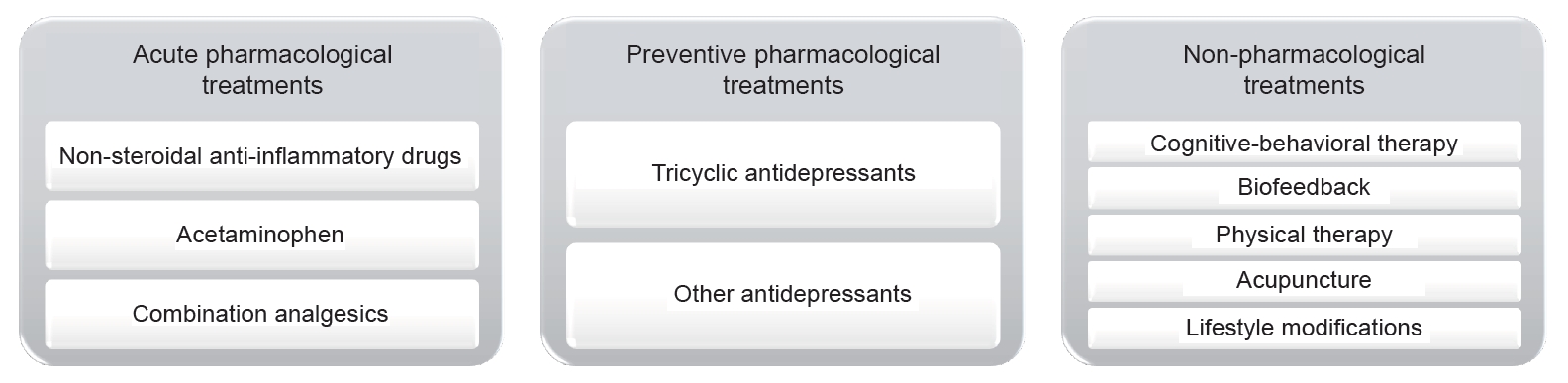
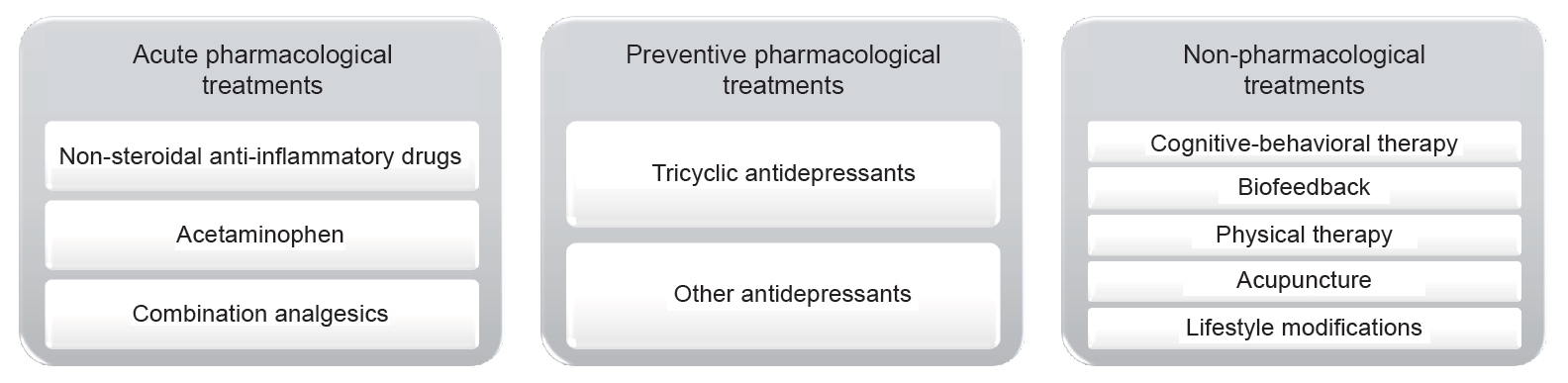
TREATMENT
• NSAIDs
• Acetaminophen
• Combination Analgesics
• Tricyclic Antidepressants (TCAs)
• Other Antidepressants
• CBT
• Biofeedback
• Physical Therapy
• Acupuncture
• Lifestyle Modifications
FUTURE RESEARCH DIRECTIONS
CONCLUSION
AVAILABILITY OF DATA AND MATERIAL
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
AUTHOR CONTRIBUTIONS
Conceptualization: HJL, SJC, JGS; Data curation: JGS, HWS; Formal analysis: JGS, HWS; Investigation: SJC; Methodology: HJL, SJC; Project administration: SJC, HWS; Resources: JGS; Software: JGS; Supervision: SJC, HWS; Validation: HJL, SJC, JGS, HWS; Visualization: HJL; Writing–original draft: HJL, SJC; Writing–review & editing: JGS, SJC, HWS.
CONFLICT OF INTEREST
Soo-Jin Cho is the Editor-in-Chief of Headache and Pain Research and was not involved in the review process of this article.
Hye Jeong Lee is the Editor of Headache and Pain Research and was not involved in the review process of this article.
Jong-Geun Seo is the Editor of Headache and Pain Research and was not involved in the review process of this article.
All authors have no other conflicts of interest to declare.
FUNDING STATEMENT
Not applicable.
ACKNOWLEDGMENTS
Not applicable.
| 2.1. Infrequent episodic tension-type headache | 2.2. Frequent episodic tension-type headache | 2.3. Chronic tension-type headache |
2.4. Probable tension-type headache |
|||
|---|---|---|---|---|---|---|
| 2.4.1. Probable infrequent episodic tension-type headache | 2.4.2. Probable frequent episodic tension-type headache | 2.4.3. Probable chronic tension-type headache | ||||
| A | At least 10 episodes of headache occurring on <1 day/mo on average (<12 days/yr) and fulfilling criteria B–D | At least 10 episodes of headache occurring on 1–14 day/mo on average for >3 months (≥12 and <180 day/yr) and fulfilling criteria B–D | Headache occurring on ≥15 day/mo on average for >3 months (≥180 day/yr), fulfilling criteria B–D | One or more episodes of headache fulfilling all but one of criteria A–D for 2.1. Infrequent episodic tension-type headache | Episodes of headache fulfilling all but one of criteria A–D for 2.2. Frequent episodic tension-type headache | Headache fulfilling all but one of criteria A–D for 2.3. Chronic episodic tension-type headache |
| B | Lasting from 30 minutes to 7 days | Lasting hours to days, or unremitting | Not fulfilling ICHD-3 criteria for any other headache disorder | |||
| C | At least two of the following four characteristics: | Not better accounted for by another ICHD-3 diagnosis | ||||
| 1. bilateral location | ||||||
| 2. pressing or tightening (non-pulsating) quality | ||||||
| 3. mild or moderate intensity | ||||||
| 4. not aggravated by routine physical activity such as walking or climbing stairs | ||||||
| D | Both of the following: | Both of the following: | ||||
| 1. no nausea or vomiting | 1. no more than one of photophobia, phonophobia or mild nausea | |||||
| 2. no more than one of photophobia or phonophobia | 2. neither moderate or severe nausea nor vomiting | |||||
| E | Not better accounted for by another ICHD-3 diagnosis1 | |||||
- 1. Turkdogan D, Cagirici S, Soylemez D, Sur H, Bilge C, Turk U. Characteristic and overlapping features of migraine and tension-type headache. Headache 2006;46:461-468.ArticlePubMed
- 2. Oguz Akarsu E, Baykan B, Ertas M, et al. The persistence versus interchangeability of migraine and tension-type headaches in a 5-year population-based validated survey. Cephalalgia 2020;40:39-48.ArticlePubMedPDF
- 3. Sahler K. Epidemiology and cultural differences in tension-type headache. Curr Pain Headache Rep 2012;16:525-532.ArticlePubMedPDF
- 4. GBD 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019;18:459-480.ArticlePubMedPMC
- 5. Deuschl G, Beghi E, Fazekas F, et al. The burden of neurological diseases in Europe: an analysis for the Global Burden of Disease Study 2017. Lancet Public Health 2020;5:e551-e567.ArticlePubMed
- 6. ; GBD 2017 US Neurological Disorders Collaborators; Feigin VL, Vos T, et al. Burden of neurological disorders across the US from 1990-2017: a global burden of disease study. JAMA Neurol 2021;78:165-176.ArticlePubMed
- 7. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1545-1602.ArticlePubMedPMC
- 8. Crystal SC, Robbins MS. Epidemiology of tension-type headache. Curr Pain Headache Rep 2010;14:449-454.ArticlePubMedPDF
- 9. Yang Y, Cao Y. Rising trends in the burden of migraine and tension-type headache among adolescents and young adults globally, 1990 to 2019. J Headache Pain 2023;24:94.ArticlePubMedPMCPDF
- 10. Rasmussen BK. Migraine and tension-type headache in a general population: precipitating factors, female hormones, sleep pattern and relation to lifestyle. Pain 1993;53:65-72.ArticlePubMed
- 11. Lyngberg AC, Rasmussen BK, Jørgensen T, Jensen R. Prognosis of migraine and tension-type headache: a population-based follow-up study. Neurology 2005;65:580-585.ArticlePubMed
- 12. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018;38:1-211.ArticlePDF
- 13. Do TP, Remmers A, Schytz HW, et al. Red and orange flags for secondary headaches in clinical practice: SNNOOP10 list. Neurology 2019;92:134-144.ArticlePubMedPMC
- 14. Onan D, Younis S, Wellsgatnik WD, et al. Debate: differences and similarities between tension-type headache and migraine. J Headache Pain 2023;24:92.ArticlePubMedPMCPDF
- 15. Buse DC, Reed ML, Fanning KM, et al. Comorbid and co-occurring conditions in migraine and associated risk of increasing headache pain intensity and headache frequency: results of the migraine in America symptoms and treatment (MAST) study. J Headache Pain 2020;21:23.ArticlePubMedPMCPDF
- 16. Kaniecki RG. Migraine and tension-type headache: an assessment of challenges in diagnosis. Neurology 2002;58:S15-S20.ArticlePubMed
- 17. Turner DP, Smitherman TA, Black AK, et al. Are migraine and tension-type headache diagnostic types or points on a severity continuum? An exploration of the latent taxometric structure of headache. Pain 2015;156:1200-1207.ArticlePubMedPMC
- 18. Ligthart L, Huijgen A, Willemsen G, de Geus EJC, Boomsma DI. Are migraine and tension-type headache genetically related? An investigation of twin family data. Twin Res Hum Genet 2018;21:112-118.ArticlePubMed
- 19. Torrente A, Maccora S, Prinzi F, et al. The clinical relevance of artificial intelligence in migraine. Brain Sci 2024;14:85.ArticlePubMedPMC
- 20. Fu GJ, Wang LD, Chi XS, et al. Research progress on the experimental model and underlying mechanistic studies of tension-type headaches. Curr Pain Headache Rep 2024;28:439-451.ArticlePubMedPMCPDF
- 21. Katsuki M, Matsumori Y, Kawamura S, et al. Developing an artificial intelligence-based diagnostic model of headaches from a dataset of clinic patients’ records. Headache 2023;63:1097-1108.ArticlePubMed
- 22. Eigenbrodt AK, Christensen RH, Ashina H, et al. Premonitory symptoms in migraine: a systematic review and meta-analysis of observational studies reporting prevalence or relative frequency. J Headache Pain 2022;23:140.ArticlePubMedPMCPDF
- 23. Nappi RE, Tiranini L, Sacco S, De Matteis E, De Icco R, Tassorelli C. Role of estrogens in menstrual migraine. Cells 2022;11:1355.ArticlePubMedPMC
- 24. Cologno D, Mazzeo A, Lecce B, et al. Triptans: over the migraine. Neurol Sci 2012;33 Suppl 1:S193-S198.ArticlePubMedPDF
- 25. Bendtsen L. Drug and nondrug treatment in tension-type headache. Ther Adv Neurol Disord 2009;2:155-161.ArticlePubMedPMCPDF
- 26. Bezov D, Ashina S, Jensen R, Bendtsen L. Pain perception studies in tension-type headache. Headache 2011;51:262-271.ArticlePubMed
- 27. Do TP, Heldarskard GF, Kolding LT, Hvedstrup J, Schytz HW. Myofascial trigger points in migraine and tension-type headache. J Headache Pain 2018;19:84.ArticlePubMedPMCPDF
- 28. Ashina M, Bendtsen L, Jensen R, Olesen J. Nitric oxide-induced headache in patients with chronic tension-type headache. Brain 2000;123:1830-1837.ArticlePubMed
- 29. Shnayder NA, Petrova MM, Moskaleva PV, Shesternya PA, Pozhilenkova EA, Nasyrova RF. The role of single-nucleotide variants of NOS1, NOS2, and NOS3 genes in the comorbidity of arterial hypertension and tension-type headache. Molecules 2021;26:1556.ArticlePubMedPMC
- 30. Repiso-Guardeño Á, Moreno-Morales N, Labajos-Manzanares MT, Rodríguez-Martínez MC, Armenta-Peinado JA. Does tension headache have a central or peripheral origin? Current state of affairs. Curr Pain Headache Rep 2023;27:801-810.ArticlePubMedPMCPDF
- 31. Jensen R, Rasmussen BK, Pedersen B, Olesen J. Muscle tenderness and pressure pain thresholds in headache. A population study. Pain 1993;52:193-199.ArticlePubMed
- 32. Jensen R, Olesen J. Initiating mechanisms of experimentally induced tension-type headache. Cephalalgia 1996;16:175-139.ArticlePubMedPDF
- 33. Aaseth K, Grande RB, Lundqvist C, Russell MB. Pericranial tenderness in chronic tension-type headache: the Akershus population-based study of chronic headache. J Headache Pain 2014;15:58.ArticlePubMedPMCPDF
- 34. Langemark M, Jensen K, Jensen TS, Olesen J. Pressure pain thresholds and thermal nociceptive thresholds in chronic tension-type headache. Pain 1989;38:203-210.ArticlePubMed
- 35. Ashina M, Bendtsen L, Jensen R, Sakai F, Olesen J. Muscle hardness in patients with chronic tension-type headache: relation to actual headache state. Pain 1999;79:201-205.ArticlePubMed
- 36. Fernández-de-Las-Peñas C, Cuadrado ML, Arendt-Nielsen L, Ge HY, Pareja JA. Increased pericranial tenderness, decreased pressure pain threshold, and headache clinical parameters in chronic tension-type headache patients. Clin J Pain 2007;23:346-352.ArticlePubMed
- 37. Del Blanco Muñiz JÁ, Sánchez Sierra A, Ladriñán Maestro A, Ucero Lozano R, Sosa-Reina MD, Martín Vera D. Cervical impairments in subjects with migraine or tension type headache: an observational study. Front Neurol 2024;15:1373912.ArticlePubMedPMC
- 38. Bendtsen L, Fernández-de-la-Peñas C. The role of muscles in tension-type headache. Curr Pain Headache Rep 2011;15:451-458.ArticlePubMedPDF
- 39. Jensen R. Peripheral and central mechanisms in tension-type headache: an update. Cephalalgia 2003;23 Suppl 1:49-52.ArticlePubMedPDF
- 40. Bendtsen L. Central sensitization in tension-type headache--possible pathophysiological mechanisms. Cephalalgia 2000;20:486-508.ArticlePubMedPDF
- 41. Chen WT, Hsiao FJ, Ko YC, et al. Comparison of somatosensory cortex excitability between migraine and “strict-criteria” tension-type headache: a magnetoencephalographic study. Pain 2018;159:793-803.ArticlePubMed
- 42. Song TJ, Cho SJ, Kim WJ, Yang KI, Yun CH, Chu MK. Anxiety and depression in tension-type headache: a population-based study. PLoS One 2016;11:e0165316.ArticlePubMedPMC
- 43. Lampl C, Thomas H, Tassorelli C, et al. Headache, depression and anxiety: associations in the Eurolight project. J Headache Pain 2016;17:59.ArticlePubMedPMCPDF
- 44. Schmidt-Wilcke T, Leinisch E, Straube A, et al. Gray matter decrease in patients with chronic tension type headache. Neurology 2005;65:1483-1486.ArticlePubMed
- 45. Chen B, He Y, Xia L, Guo LL, Zheng JL. Cortical plasticity between the pain and pain-free phases in patients with episodic tension-type headache. J Headache Pain 2016;17:105.ArticlePubMedPMCPDF
- 46. Bendtsen L, Evers S, Linde M, et al. EFNS guideline on the treatment of tension-type headache: report of an EFNS task force. Eur J Neurol 2010;17:1318-1325.ArticlePubMed
- 47. Moore RA, Derry S, Wiffen PJ, Straube S, Bendtsen L. Evidence for efficacy of acute treatment of episodic tension-type headache: methodological critique of randomised trials for oral treatments. Pain 2014;155:2220-2228.ArticlePubMed
- 48. Lenaerts ME. Pharmacotherapy of tension-type headache (TTH). Expert Opin Pharmacother 2009;10:1261-1271.ArticlePubMed
- 49. Derry S, Wiffen PJ, Moore RA, Bendtsen L. Ibuprofen for acute treatment of episodic tension-type headache in adults. Cochrane Database Syst Rev 2015;2015:CD011474.ArticlePubMedPMC
- 50. Veys L, Derry S, Moore RA. Ketoprofen for episodic tension-type headache in adults. Cochrane Database Syst Rev 2016;9:CD012190.ArticlePubMed
- 51. Stephens G, Derry S, Moore RA. Paracetamol (acetaminophen) for acute treatment of episodic tension-type headache in adults. Cochrane Database Syst Rev 2016;2016:CD011889.ArticlePubMedPMC
- 52. Diener HC, Gold M, Hagen M. Use of a fixed combination of acetylsalicylic acid, acetaminophen and caffeine compared with acetaminophen alone in episodic tension-type headache: meta-analysis of four randomized, double-blind, placebo-controlled, crossover studies. J Headache Pain 2014;15:76.ArticlePubMedPMCPDF
- 53. Lipton RB, Diener HC, Robbins MS, Garas SY, Patel K. Caffeine in the management of patients with headache. J Headache Pain 2017;18:107.ArticlePubMedPMCPDF
- 54. Krøll LS, Callesen HE, Carlsen LN, et al. Manual joint mobilisation techniques, supervised physical activity, psychological treatment, acupuncture and patient education for patients with tension-type headache. A systematic review and meta-analysis. J Headache Pain 2021;22:96.ArticlePubMedPMC
- 55. Christiansen S, Jürgens TP, Klinger R. Outpatient combined group and individual cognitive-behavioral treatment for patients with migraine and tension-type headache in a routine clinical setting. Headache 2015;55:1072-1091.ArticlePubMed
- 56. Holroyd KA, O’Donnell FJ, Stensland M, Lipchik GL, Cordingley GE, Carlson BW. Management of chronic tension-type headache with tricyclic antidepressant medication, stress management therapy, and their combination: a randomized controlled trial. JAMA 2001;285:2208-2215.ArticlePubMedPMC
- 57. Andrasik F, Grazzi L, Sansone E, D’Amico D, Raggi A, Grignani E. Non-pharmacological approaches for headaches in young age: an updated review. Front Neurol 2018;9:1009.ArticlePubMedPMC
- 58. Andrasik F, Grazzi L, Usai S, Bussone G. Pharmacological treatment compared to behavioural treatment for juvenile tension-type headache: results at two-year follow-up. Neurol Sci 2007;28 Suppl 2:S235-S238.ArticlePubMedPDF
- 59. Luedtke K, Allers A, Schulte LH, May A. Efficacy of interventions used by physiotherapists for patients with headache and migraine-systematic review and meta-analysis. Cephalalgia 2016;36:474-492.ArticlePubMedPDF
- 60. Repiso-Guardeño A, Moreno-Morales N, Armenta-Pendón MA, Rodríguez-Martínez MDC, Pino-Lozano R, Armenta-Peinado JA. Physical therapy in tension-type headache: a systematic review of randomized controlled trials. Int J Environ Res Public Health 2023;20:4466.ArticlePubMedPMC
- 61. Cumplido-Trasmonte C, Fernández-González P, Alguacil-Diego IM, Molina-Rueda F. Manual therapy in adults with tension-type headache: a systematic review. Neurologia (Engl Ed) 2021;36:537-547.ArticlePubMed
- 62. Lu L, Wen Q, Hao X, Zheng Q, Li Y, Li N. Acupoints for tension-type headache: a literature study based on data mining technology. Evid Based Complement Alternat Med 2021;2021:5567697.ArticlePubMedPMCPDF
- 63. Chowdhury D, Datta D, Mundra A. Role of greater occipital nerve block in headache disorders: a narrative review. Neurol India 2021;69:S228-S256.ArticlePubMed
- 64. Kim JY, Choo YJ, Chang MC. Ultrasound-guided 5-in-1 trigger point injection for treating tension-type headache: a case report. Medicine (Baltimore) 2022;101:e29987.ArticlePubMedPMC
- 65. Cho SJ. When should headache specialists hold a needle? The role of botulinum toxin injections and occipital nerve blocks. Headache Pain Res 2024;25:73-74.Article
- 66. Linde K, Allais G, Brinkhaus B, et al. Acupuncture for the prevention of tension-type headache. Cochrane Database Syst Rev 2016;4:CD007587.ArticlePubMed
- 67. Gonçalves DA, Bigal ME, Jales LC, Camparis CM, Speciali JG. Headache and symptoms of temporomandibular disorder: an epidemiological study. Headache 2010;50:231-241.ArticlePubMed
- 68. Bigal ME, Lipton RB. Modifiable risk factors for migraine progression (or for chronic daily headaches): clinical lessons. Headache 2006;46 Suppl 3:S144-S146.ArticlePubMed
- 69. Ashina S, Mitsikostas DD, Lee MJ, et al. Tension-type headache. Nat Rev Dis Primers 2021;7:24.ArticlePubMedPDF
REFERENCES
Figure & Data
References
Citations

- Tension-Type Headache in Brazzaville: Prevalence and Sociodemographic Profile from a Cross-Sectional Population-Based Study
Ghislain Armel Mpandzou, Dinah Happhia Motoula Latou, Amedna Madh Beny Koukat, Prince Eliot Galiéni Sounga Bandzouzi, Josué Euberma Diatewa, Yacouba Kaba, Karen Lise Obondzo Aloba, Paul Macaire Ossou-Nguiet
World Journal of Neuroscience.2026; 16(01): 57. CrossRef - Tension-Type Headache and Primary Stabbing Headache: Primary Headaches Beyond Migraine
Mi-Kyoung Kang
Headache and Pain Research.2025; 26(2): 89. CrossRef - Hallmarks of primary headache: part 2– Tension-type headache
Li-Ling Hope Pan, Yu-Hsiang Ling, Shuu-Jiun Wang, Linda Al-Hassany, Wei-Ta Chen, Chia-Chun Chiang, Soo-Jin Cho, Min Kyung Chu, Gianluca Coppola, Adriana Della Pietra, Zhao Dong, Esme Ekizoglu, Charl Els, Fatemeh Farham, David Garcia-Azorin, Woo-Seok Ha, F
The Journal of Headache and Pain.2025;[Epub] CrossRef - Trends in the Burden of Headache Disorders in Europe, 1990–2021: A Systematic Analysis from the Global Burden of Disease Study 2021
Terry Jung, Yoonkyung Chang, Moon-Kyung Shin, Sohee Wang, Seyedehmahla Hosseini, Joonho Kim, Min Kyung Chu, Tae-Jin Song
Journal of Clinical Medicine.2025; 14(19): 6966. CrossRef - Interoception Accuracy Differences in Patients with Chronic Tension-type Headache
İnan Özdemir, Güllüşah Üstün, Serkan Aksu, Semai Bek, Gülnihal Kutlu
Neurological Sciences and Neurophysiology.2025; 42(3): 116. CrossRef - Results of the observational program CITOTREK (use of the drug CITOflavin in Tablets) in patients with tension headaches against the backgRound of asthenic syndromE taKing into account comorbidity
M.V. Putilina, N.I. Shabalina, I.A. Blinova
S.S. Korsakov Journal of Neurology and Psychiatry.2025; 125(10): 104. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
- Related articles
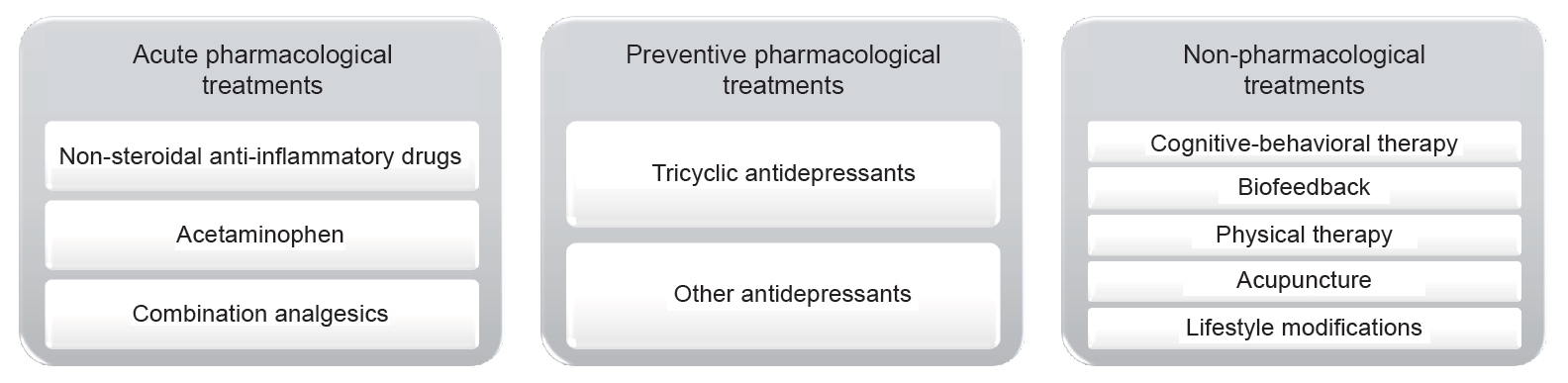
Figure 1.
| 2.1. Infrequent episodic tension-type headache | 2.2. Frequent episodic tension-type headache | 2.3. Chronic tension-type headache | 2.4. Probable tension-type headache |
|||
|---|---|---|---|---|---|---|
| 2.4.1. Probable infrequent episodic tension-type headache | 2.4.2. Probable frequent episodic tension-type headache | 2.4.3. Probable chronic tension-type headache | ||||
| A | At least 10 episodes of headache occurring on <1 day/mo on average (<12 days/yr) and fulfilling criteria B–D | At least 10 episodes of headache occurring on 1–14 day/mo on average for >3 months (≥12 and <180 day/yr) and fulfilling criteria B–D | Headache occurring on ≥15 day/mo on average for >3 months (≥180 day/yr), fulfilling criteria B–D | One or more episodes of headache fulfilling all but one of criteria A–D for 2.1. Infrequent episodic tension-type headache | Episodes of headache fulfilling all but one of criteria A–D for 2.2. Frequent episodic tension-type headache | Headache fulfilling all but one of criteria A–D for 2.3. Chronic episodic tension-type headache |
| B | Lasting from 30 minutes to 7 days | Lasting hours to days, or unremitting | Not fulfilling ICHD-3 criteria for any other headache disorder | |||
| C | At least two of the following four characteristics: | Not better accounted for by another ICHD-3 diagnosis | ||||
| 1. bilateral location | ||||||
| 2. pressing or tightening (non-pulsating) quality | ||||||
| 3. mild or moderate intensity | ||||||
| 4. not aggravated by routine physical activity such as walking or climbing stairs | ||||||
| D | Both of the following: | Both of the following: | ||||
| 1. no nausea or vomiting | 1. no more than one of photophobia, phonophobia or mild nausea | |||||
| 2. no more than one of photophobia or phonophobia | 2. neither moderate or severe nausea nor vomiting | |||||
| E | Not better accounted for by another ICHD-3 diagnosis1 | |||||
Table 1.
TOP
 KHS
KHS