Articles
- Page Path
- HOME > Headache Pain Res > Volume 25(1); 2024 > Article
-
Original Article
Associations of Migraine and Tension-type Headache with Glaucoma -
Jong-Ho Kim1,2
 , Young-Suk Kwon1,2
, Young-Suk Kwon1,2 , Sang-Hwa Lee2,3
, Sang-Hwa Lee2,3 , Jong-Hee Sohn2,3
, Jong-Hee Sohn2,3
-
Headache and Pain Research 2024;25(1):54-62.
DOI: https://doi.org/10.62087/hpr.2024.0002
Published online: March 29, 2024
1Department of Anesthesiology and Pain Medicine, Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Republic of Korea
2Institute of New Frontier Research Team, Hallym University College of Medicine, Chuncheon, Republic of Korea
3Department of Neurology, Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Republic of Korea
- Corresponding for author: Jong-Hee Sohn, M.D., Ph.D. Department of Neurology, Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, 77 Sakju-ro, Chuncheon 24253, Republic of Korea Tel: +82-33-240-5255, Fax: +82-33-241-8063, E-mail: deepfoci@hallym.or.kr
© 2024 The Korean Headache Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 5,476 Views
- 65 Download
- 4 Crossref
Abstract
-
Purpose
- It remains unclear whether primary headaches, particularly migraine, are associated with glaucoma. We investigated potential associations between primary headaches, including migraine and tension-type headache (TTH), and primary glaucoma, including open-angle glaucoma (OAG) and closed-angle glaucoma (CAG).
-
Methods
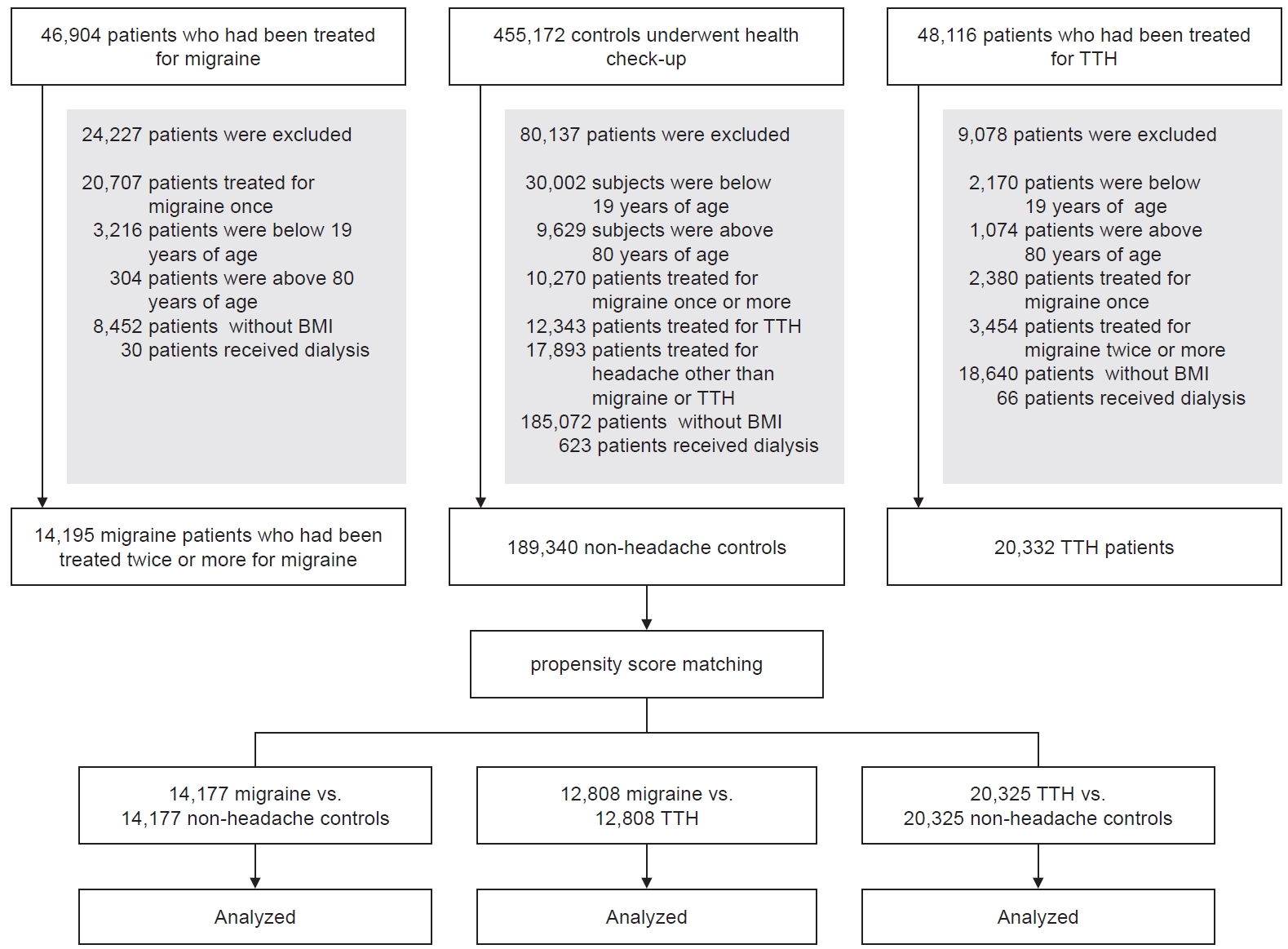
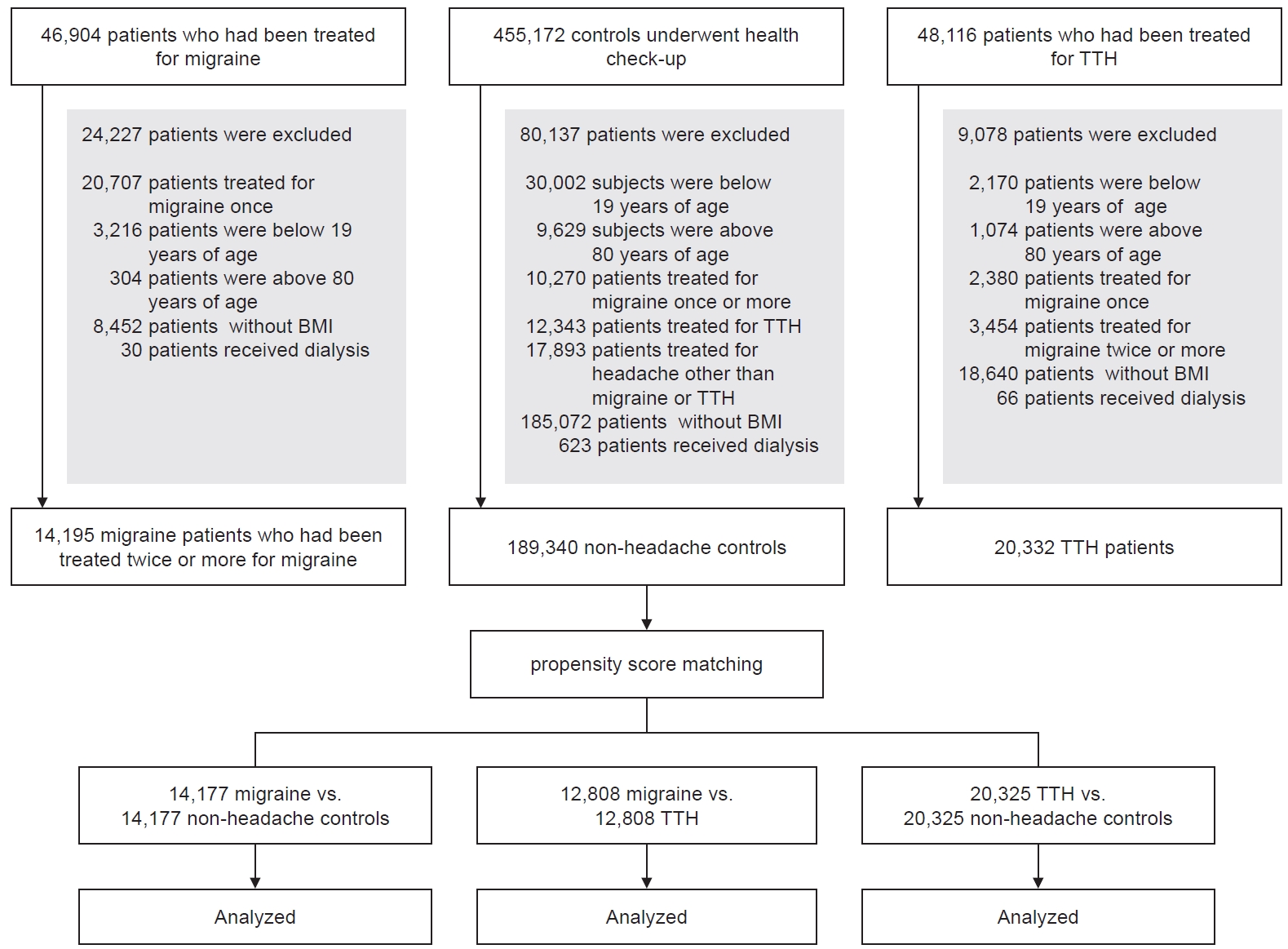
- We used data from the Clinical Data Warehouse collected between 2008 and 2023 to investigate whether migraine and TTH influence the risk of primary glaucoma. We compared the prevalence of primary glaucoma, including OAG, CAG, other glaucoma, and total glaucoma (TG), among patients with migraine, those with TTH, and controls.
-
Results
- This study analyzed 46,904 patients with migraine, 48,116 patients with TTH, and 455,172 controls. Controls were selected based on propensity score matching (PSM). After adjustment for covariates and PSM, the fully adjusted odds ratios (ORs) for patients with migraine were 1.83 for OAG (95% confidence interval [95% CI], 1.33–2.51; p<0.004) and 1.55 for TG (95% CI, 1.26–1.91; p<0.004) compared to controls. Furthermore, in patients with TTH, the ORs for CAG were 2.20 (95% CI, 1.40–3.47; p<0.004) compared to controls. Additionally, patients with migraine had fully adjusted ORs of 1.71 for OAG (95% CI, 1.24–2.36; p<0.004) and 1.41 for TG (95% CI, 1.15–1.73; p<0.004) compared to those with TTH.
-
Conclusion
- Migraine is associated with primary glaucoma, particularly OAG.
INTRODUCTION
MATERIALS AND METHODS
RESULTS
DISCUSSION
Availability of data and material
The data presented in this study are available upon reasonable request from the corresponding author.
Author contributions
Conceptualization: SHL, JHS; Data curation: JHK, YSK; Formal analysis: JHK; Investigation: JHK, JHS; Methodology: JHK, JHS; Software: JHK, JHS; Validation: JHK, JHS; Writing–original draft: JHK, JHS; Writing–review and editing: all authors.
All authors have read and agreed to the published version of the manuscript.
Conflict of interest
Jong-Hee Sohn is the Editor of Headache and Pain Research and was not involved in the review process of this article. All authors have no other conflicts of interest to declare.
Funding statement
This research was supported by “Physician scientist training and future medical technology implementation for solving clinical challenges in nervous system” (RS-2023-00223501). The role of funding was in the design of the study and collection, analysis, and interpretation of data. No other financial relationships relevant to this publication were disclosed.
Acknowledgments
Not applicable.
Values are presented as number (%) or mean±standard deviation.
ASD, absolute standardized difference; BMI, body mass index; DM, diabetes mellitus; HTN, hypertension; AF, atrial fibrillation; CVD, cerebrovascular disease; OAG, open-angle glaucoma; CAG, closed-angle glaucoma; OG, other glaucoma; TG, total glaucoma.
Values are presented as number (%) or mean±standard deviation.
TTH, tension-type headache; ASD, absolute standardized difference; BMI, body mass index; DM, diabetes mellitus; HTN, hypertension; AF, atrial fibrillation; CVD, cerebrovascular disease; OAG, open-angle glaucoma; CAG, closed-angle glaucoma; OG, other glaucoma; TG, total glaucoma.
Values are presented as number (%) or mean±standard deviation.
TTH, tension-type headache; ASD, absolute standardized difference; BMI, body mass index; DM, diabetes mellitus; HTN, hypertension; AF, atrial fibrillation; CVD, cerebrovascular disease ; OAG, open-angle glaucoma; CAG, closed-angle glaucoma; OG, other glaucoma; TG, total glaucoma.
*Asterisk indicates a statistically significant (p<0.004).
OR, odds ratio; TTH, tension-type headache; CI, confidence interval; UA, unadjusted; AVA, all variables adjusted; AVPA, all variables plus propensity score adjusted; OAG, open-angle glaucoma; CAG, closed-angle glaucoma; OG, other glaucoma; TG, total glaucoma.
*Asterisk indicates a statistically significant (p<0.004).
OR, odds ratio; TTH, tension-type headache; CI, confidence interval; UA, unadjusted; AVA, all variables adjusted; AVPA, all variables plus propensity score adjusted; OAG, open-angle glaucoma; CAG, closed-angle glaucoma; OG, other glaucoma; TG, total glaucoma.
- 1. Tietjen EG. Migraine and ischaemic heart disease and stroke: potential mechanisms and treatment implications. Cephalalgia 2007;27:981-987.ArticlePubMedPDF
- 2. Pietrobon D, Moskowitz MA. Pathophysiology of migraine. Annu Rev Physiol 2013;75:365-391.ArticlePubMed
- 3. Larrosa-Campo D, Ramón-Carbajo C, Para-Prieto M, Calleja-Puerta S, Cernuda-Morollón E, Pascual J. Migraine as a vascular risk factor. Rev Neurol 2012;55:349-358. Spanish.ArticlePubMed
- 4. Bigal ME, Kurth T, Hu H, Santanello N, Lipton RB. Migraine and cardiovascular disease: possible mechanisms of interaction. Neurology 2009;72:1864-1871.ArticlePubMedPMC
- 5. Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 2014;121:2081-2090.ArticlePubMed
- 6. Resnikoff S, Pascolini D, Etya’ale D, et al. Global data on visual impairment in the year 2002. Bull World Health Organ 2004;82:844-851.PubMedPMC
- 7. Chen HY, Chang YC, Wang IJ, Chen WC. Comparison of glaucoma diagnoses using Stratus and Cirrus optical coherence tomography in different glaucoma types in a Chinese population. J Glaucoma 2013;22:638-646.ArticlePubMed
- 8. Chen HY, Chang YC, Chen WC, Lane HY. Association between plasma endothelin-1 and severity of different types of glaucoma. J Glaucoma 2013;22:117-122.ArticlePubMed
- 9. Bonomi L, Marchini G, Marraffa M, Bernardi P, Morbio R, Varotto A. Vascular risk factors for primary open angle glaucoma: the Egna-Neumarkt Study. Ophthalmology 2000;107:1287-1293.ArticlePubMed
- 10. Kim C, Kim TW. Comparison of risk factors for bilateral and unilateral eye involvement in normal-tension glaucoma. Invest Ophthalmol Vis Sci 2009;50:1215-1220.ArticlePubMed
- 11. Yanagi M, Kawasaki R, Wang JJ, Wong TY, Crowston J, Kiuchi Y. Vascular risk factors in glaucoma: a review. Clin Exp Ophthalmol 2011;39:252-258.ArticlePubMed
- 12. Chen HY, Lin CL. Comparison of medical comorbidity between patients with primary angle-closure glaucoma and a control cohort: a population-based study from Taiwan. BMJ Open 2019;9:e024209.ArticlePubMedPMC
- 13. Ohn K, Han K, Moon JI, Jung Y. Presence and severity of migraine is associated with development of primary open angle glaucoma: a population-based longitudinal cohort study. PLoS One 2023;18:e0283495.ArticlePubMedPMC
- 14. Huang JY, Su CC, Wang TH, Tsai IJ. Migraine and increased risk of developing open angle glaucoma: a population-based cohort study. BMC Ophthalmol 2019;19:50.ArticlePubMedPMCPDF
- 15. Chen HY, Lin CL, Kao CH. Does migraine increase the risk of glaucoma?: a population-based cohort study. Medicine (Baltimore) 2016;95:e3670.ArticlePubMedPMC
- 16. Wang JJ, Mitchell P, Smith W. Is there an association between migraine headache and open-angle glaucoma? Findings from the Blue Mountains Eye Study. Ophthalmology 1997;104:1714-1719.ArticlePubMed
- 17. Lin HC, Chien CW, Hu CC, Ho JD. Comparison of comorbid conditions between open-angle glaucoma patients and a control cohort: a case-control study. Ophthalmology 2010;117:2088-2095.ArticlePubMed
- 18. Lin HC, Kang JH, Jiang YD, Ho JD. Hypothyroidism and the risk of developing open-angle glaucoma: a five-year population-based follow-up study. Ophthalmology 2010;117:1960-1966.ArticlePubMed
- 19. Landers J, Goldberg I, Graham SL. Analysis of risk factors that may be associated with progression from ocular hypertension to primary open angle glaucoma. Clin Exp Ophthalmol 2002;30:242-247.ArticlePubMedPDF
- 20. Xu C, Li J, Li Z, Mao X. Migraine as a risk factor for primary open angle glaucoma: a systematic review and meta-analysis. Medicine (Baltimore) 2018;97:e11377.ArticlePubMedPMC
- 21. Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA 2014;311:1901-1911.ArticlePubMedPMC
- 22. Dalkara T, Nozari A, Moskowitz MA. Migraine aura pathophysiology: the role of blood vessels and microembolisation. Lancet Neurol 2010;9:309-317.ArticlePubMedPMC
- 23. Harris A, Harris M, Biller J, et al. Aging affects the retrobulbar circulation differently in women and men. Arch Ophthalmol 2000;118:1076-1080.ArticlePubMed
- 24. Flammer J, Pache M, Resink T. Vasospasm, its role in the pathogenesis of diseases with particular reference to the eye. Prog Retin Eye Res 2001;20:319-349.ArticlePubMed
- 25. Pache M, Flammer J. A sick eye in a sick body? Systemic findings in patients with primary open-angle glaucoma. Surv Ophthalmol 2006;51:179-212.ArticlePubMed
- 26. Werne A, Harris A, Moore D, BenZion I, Siesky B. The circadian variations in systemic blood pressure, ocular perfusion pressure, and ocular blood flow: risk factors for glaucoma? Surv Ophthalmol 2008;53:559-567.ArticlePubMed
- 27. Costa VP, Harris A, Anderson D, et al. Ocular perfusion pressure in glaucoma. Acta Ophthalmol 2014;92:e252-e266.ArticlePubMed
- 28. Nesher R, Mimouni MD, Khoury S, Nesher G, Segal O. Delayed diagnosis of subacute angle closure glaucoma in patients presenting with headaches. Acta Neurol Belg 2014;114:269-272.ArticlePubMedPDF
- 29. Nesher R, Epstein E, Stern Y, Assia E, Nesher G. Headaches as the main presenting symptom of subacute angle closure glaucoma. Headache 2005;45:172-176.ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- The association between migraine and glaucoma diseases: A retrospective cohort study
Matan Bar, Ido Peles, Gal Ifergane, Erez Tsumi, Assaf Kratz
Headache: The Journal of Head and Face Pain.2026; 66(1): 144. CrossRef - Exploring Secondary Headaches: Insights from Glaucoma and COVID-19 Infection
Soo-Kyoung Kim
Headache and Pain Research.2025; 26(1): 3. CrossRef - Association between migraine and primary open-angle glaucoma: A two-sample Mendelian randomization study
Dima L Chaar, Aliya Yakubova, Chen Jiang, Thomas J Hoffmann, Alice Pressman, Denis Plotnikov, Hélène Choquet
Cephalalgia Reports.2025;[Epub] CrossRef - Subjective Cognitive Decline Patterns in Patients with Migraine, with or without Depression, versus Non-depressed Older Adults
Sun Hwa Lee, Soo-Jin Cho
Headache and Pain Research.2024; 25(2): 103. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
- Related articles
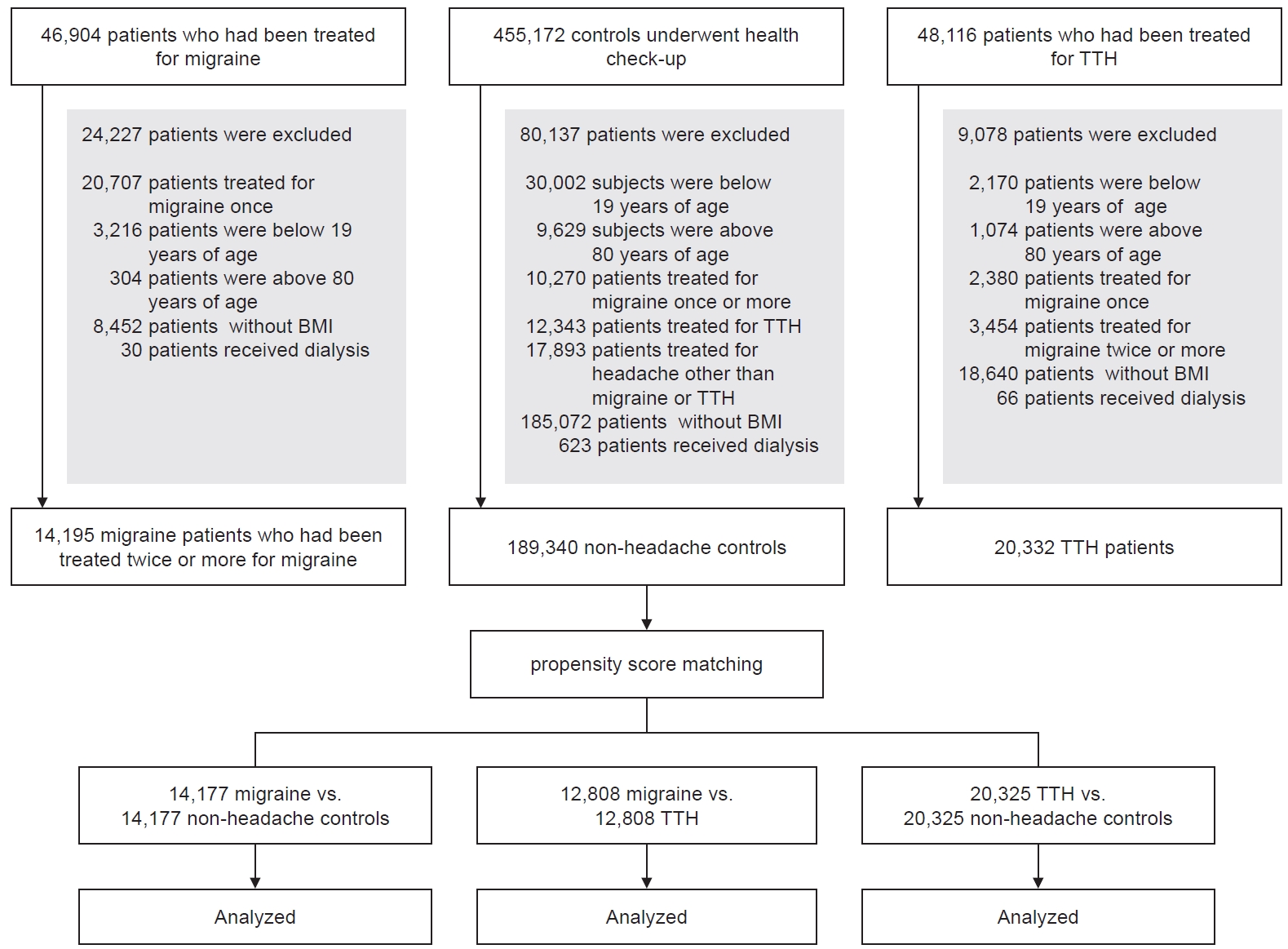
Figure 1.
| Before matching | After matching | |||||
|---|---|---|---|---|---|---|
| Migraine (n=14,195) | Control (n=189,340) | ASD | Migraine (n=14,177) | Control (n=14,177) | ASD | |
| Female sex | 10,523 (74.1) | 91,309 (48.2) | 0.59 | 10,505 (74.1) | 10,619 (74.9) | 0.02 |
| Age (yr) | 45.6±14.4 | 49.8±14.7 | 0.30 | 45.6±14.4 | 46.1±14.8 | 0.03 |
| BMI (kg/m2) | 23.8±4.0 | 24.2±3.7 | 0.09 | 23.8±4.0 | 23.8±4.0 | 0.00 |
| DM | 1,045 (7.4) | 19,468 (10.3) | 0.11 | 1,043 (7.4) | 985 (6.9) | 0.02 |
| HTN | 2,378 (16.8) | 28,802 (15.2) | 0.04 | 2,370 (16.7) | 2,378 (16.8) | 0.00 |
| Dyslipidemia | 1,956 (13.8) | 25,512 (13.5) | 0.01 | 1,950 (13.8) | 2,010 (14.2) | 0.01 |
| Angina | 1,226 (8.6) | 1,2951 (6.8) | 0.06 | 1,218 (8.6) | 1,277 (9.0) | 0.01 |
| AF | 170 (1.2) | 4,092 (2.2) | 0.09 | 170 (1.2) | 173 (1.2) | 0.00 |
| Heart disease | 951 (6.7) | 12,517 (6.6) | 0.00 | 949 (6.7) | 946 (6.7) | 0.00 |
| CVD | 2,647 (18.6) | 17,666 (9.3) | 0.24 | 2,631 (18.6) | 2,632 (18.6) | 0.00 |
| Chronic pulmonary disease | 1,538 (10.8) | 17,294 (9.1) | 0.05 | 1,529 (10.8) | 1,494 (10.5) | 0.01 |
| Renal failure | 270 (1.9) | 5,007 (2.6) | 0.05 | 269 (1.9) | 284 (2.0) | 0.01 |
| Chronic hepatitis | 538 (3.8) | 13,205 (7.0) | 0.17 | 538 (3.8) | 493 (3.5) | 0.02 |
| Anxiety | 782 (5.5) | 3,543 (1.9) | 0.16 | 771 (5.4) | 765 (5.4) | 0.00 |
| Depression | 2,003 (14.1) | 7,756 (4.1) | 0.29 | 1,985 (14.0) | 2,024 (14.3) | 0.01 |
| Sleep disorder | 1,413 (10.0) | 5,996 (3.2) | 0.23 | 1,397 (9.9) | 1,385 (9.8) | 0.00 |
| Menopause | 834 (5.9) | 7,517 (4.0) | 0.08 | 831 (5.9) | 863 (6.1) | 0.01 |
| OAG | 106 (0.7) | 912 (0.5) | 106 (0.7) | 61 (0.4) | ||
| CAG | 23 (0.2) | 183 (0.1) | 23 (0.2) | 10 (0.1) | ||
| OG | 122 (0.9) | 1,446 (0.8) | 122 (0.9) | 118 (0.8) | ||
| TG | 229 (1.6) | 2,182 (1.2) | 229 (1.6) | 158 (1.1) | ||
| Before matching | After matching | |||||
|---|---|---|---|---|---|---|
| TTH (n=20,332) | Control (n=189,340) | ASD | TTH (n=20,325) | Control (n=20,325) | ASD | |
| Female sex | 12,344 (60.7) | 91,309 (48.2) | 0.26 | 12,337 (60.7) | 12,416 (61.1) | 0.01 |
| Age (yr) | 52.8±13.7 | 49.8±14.7 | 0.22 | 52.8±13.7 | 53.3±14.3 | 0.04 |
| BMI (kg/m2) | 24.3±3.5 | 24.2±3.7 | 0.05 | 24.3±3.5 | 24.4±3.7 | 0.01 |
| DM | 2,420 (11.9) | 19,468 (10.3) | 0.05 | 2,419 (11.9) | 2,361 (11.6) | 0.01 |
| HTN | 4,996 (24.6) | 28,802 (15.2) | 0.22 | 4,990 (24.6) | 5,074 (25.0) | 0.01 |
| Dyslipidemia | 3,800 (18.7) | 25,512 (13.5) | 0.13 | 3,794 (18.7) | 3,624 (17.8) | 0.02 |
| Angina | 2,647 (13.0) | 12,951 (6.8) | 0.18 | 2,640 (13.0) | 2,592 (12.8) | 0.01 |
| AF | 578 (2.8) | 4,092 (2.2) | 0.04 | 578 (2.8) | 575 (2.8) | 0.00 |
| Heart disease | 2,017 (9.9) | 12,517 (6.6) | 0.11 | 2,015 (9.9) | 1,934 (9.5) | 0.01 |
| CVD | 4,322 (21.3) | 17,666 (9.3) | 0.29 | 4,315 (21.2) | 4,438 (21.8) | 0.01 |
| Chronic pulmonary disease | 3,100 (15.2) | 17,294 (9.1) | 0.17 | 3,095 (15.2) | 3,172 (15.6) | 0.01 |
| Renal failure | 644 (3.2) | 5,007 (2.6) | 0.03 | 644 (3.2) | 605 (3.0) | 0.01 |
| Chronic hepatitis | 1,220 (6.0) | 13,205 (7.0) | 0.04 | 1,217 (6.0) | 1,200 (5.9) | 0.00 |
| Anxiety | 1,326 (6.5) | 3,543 (1.9) | 0.19 | 1,319 (6.5) | 1,199 (5.9) | 0.02 |
| Depression | 2,374 (11.7) | 7,756 (4.1) | 0.24 | 2,368 (11.7) | 2,227 (11.0) | 0.02 |
| Sleep disorder | 1,574 (7.7) | 5,996 (3.2) | 0.17 | 1,567 (7.7) | 1,450 (7.1) | 0.02 |
| Menopause | 1,555 (7.6) | 7,517 (4.0) | 0.14 | 1,548 (7.6) | 1,610 (7.9) | 0.01 |
| OAG | 144 (0.7) | 912 (0.5) | 144 (0.7) | 99 (0.5) | ||
| CAG | 58 (0.3) | 183 (0.1) | 58 (0.3) | 28 (0.1) | ||
| OG | 215 (1.1) | 1,446 (0.8) | 215 (1.1) | 211 (1.0) | ||
| TG | 353 (1.7) | 2,182 (1.2) | 353 (1.7) | 294 (1.4) | ||
| Before matching | After matching | |||||
|---|---|---|---|---|---|---|
| Migraine (n=14,195) | TTH (n=20,332) | ASD | Migraine (n=12,808) | TTH (n=12,808) | ASD | |
| Female sex | 10,523 (74.1) | 12,344 (60.7) | 0.31 | 9,192 (71.8) | 8,974 (70.1) | 0.04 |
| Age (yr) | 45.6±14.4 | 52.8±13.7 | 0.50 | 47.1±14.1 | 48.3±13.2 | 0.08 |
| BMI (kg/m2) | 23.8±4.0 | 24.3±3.5 | 0.14 | 24.0±3.9 | 24.0±3.5 | 0.02 |
| DM | 1,045 (7.4) | 2,420 (11.9) | 0.17 | 1,018 (7.9) | 1,100 (8.6) | 0.02 |
| HTN | 2,378 (16.8) | 4,996 (24.6) | 0.21 | 2,316 (18.1) | 2,416 (18.9) | 0.02 |
| Dyslipidemia | 1,956 (13.8) | 3,800 (18.7) | 0.14 | 1,904 (14.9) | 1,955 (15.3) | 0.01 |
| Angina | 1,226 (8.6) | 2,647 (13.0) | 0.16 | 1,191 (9.3) | 1,243 (9.7) | 0.01 |
| AF | 170 (1.2) | 578 (2.8) | 0.15 | 170 (1.3) | 189 (1.5) | 0.01 |
| Heart disease | 951 (6.7) | 2,017 (9.9) | 0.13 | 915 (7.1) | 929 (7.3) | 0.00 |
| CVD | 2,647 (18.6) | 4,322 (21.3) | 0.07 | 2,477 (19.3) | 2,528 (19.7) | 0.01 |
| Chronic pulmonary disease | 1,538 (10.8) | 3,100 (15.2) | 0.14 | 1,449 (11.3) | 1,475 (11.5) | 0.01 |
| Renal failure | 270 (1.9) | 644 (3.2) | 0.09 | 265 (2.1) | 300 (2.3) | 0.02 |
| Chronic hepatitis | 538 (3.8) | 1,220 (6.0) | 0.12 | 529 (4.1) | 540 (4.2) | 0.00 |
| Anxiety | 782 (5.5) | 1,326 (6.5) | 0.04 | 732 (5.7) | 760 (5.9) | 0.01 |
| Depression | 2,003 (14.1) | 2,374 (11.7) | 0.07 | 1,759 (13.7) | 1,705 (13.3) | 0.01 |
| Sleep disorder | 1,413 (10.0) | 1,574 (7.7) | 0.07 | 1,197 (9.3) | 1,185 (9.3) | 0.00 |
| Menopause | 834 (5.9) | 1,555 (7.6) | 0.08 | 824 (6.4) | 878 (6.9) | 0.02 |
| OAG | 106 (0.7) | 144 (0.7) | 101 (0.8) | 61 (0.5) | ||
| CAG | 23 (0.2) | 58 (0.3) | 23 (0.2) | 21 (0.2) | ||
| OG | 122 (0.9) | 215 (1.1) | 118 (0.9) | 103 (0.8) | ||
| TG | 229 (1.6) | 353 (1.7) | 220 (1.7) | 163 (1.3) | ||
| OR (95% CI) | ||||
|---|---|---|---|---|
| OAG | CAG | OG | TG | |
| UA | 1.74* (1.27–2.39) | 2.30 (1.10–4.84) | 1.03 (0.80–1.33) | 1.46* (1.19–1.79) |
| AVA | 1.83* (1.33–2.51) | 2.55 (1.21–5.39) | 1.10 (0.85–1.43) | 1.55* (1.26–1.91) |
| AVPA | 1.83* (1.33–2.51) | 2.55 (1.21–5.39) | 1.10 (0.85–1.43) | 1.55* (1.26–1.91) |
| OR (95% CI) | ||||
|---|---|---|---|---|
| OAG | CAG | OG | TG | |
| UA | 1.46 (1.13–1.88) | 2.07* (1.32–3.26) | 1.02 (0.84–1.23) | 1.20 (1.03–1.41) |
| AVA | 1.53 (1.18–1.98) | 2.20* (1.40–3.46) | 1.07 (0.89–1.30) | 1.27* (1.08-1.48) |
| AVPA | 1.53 (1.18–1.98) | 2.20* (1.40–3.47) | 1.08 (0.89–1.30) | 1.27* (1.08–1.48) |
| OR (95% CI) | ||||
|---|---|---|---|---|
| OAG | CAG | OG | TG | |
| UA | 1.66* (1.21–2.28) | 1.10 (0.61–1.98) | 1.15 (0.88–1.50) | 1.36* (1.11–1.66) |
| AVA | 1.72 (1.25–2.37) | 1.12 (0.62–2.02) | 1.19 (0.91–1.55) | 1.40* (1.14–1.73) |
| AVPA | 1.71* (1.24–2.36) | 1.12 (0.62–2.03) | 1.19 (0.91–1.56) | 1.41* (1.15–1.73) |
Values are presented as number (%) or mean±standard deviation. ASD, absolute standardized difference; BMI, body mass index; DM, diabetes mellitus; HTN, hypertension; AF, atrial fibrillation; CVD, cerebrovascular disease; OAG, open-angle glaucoma; CAG, closed-angle glaucoma; OG, other glaucoma; TG, total glaucoma.
Values are presented as number (%) or mean±standard deviation. TTH, tension-type headache; ASD, absolute standardized difference; BMI, body mass index; DM, diabetes mellitus; HTN, hypertension; AF, atrial fibrillation; CVD, cerebrovascular disease; OAG, open-angle glaucoma; CAG, closed-angle glaucoma; OG, other glaucoma; TG, total glaucoma.
Values are presented as number (%) or mean±standard deviation. TTH, tension-type headache; ASD, absolute standardized difference; BMI, body mass index; DM, diabetes mellitus; HTN, hypertension; AF, atrial fibrillation; CVD, cerebrovascular disease ; OAG, open-angle glaucoma; CAG, closed-angle glaucoma; OG, other glaucoma; TG, total glaucoma.
*Asterisk indicates a statistically significant (p<0.004). OR, odds ratio; CI, confidence interval; UA, unadjusted; AVA, all variables adjusted; AVPA, all variables plus propensity score adjusted; OAG, open-angle glaucoma; CAG, closed-angle glaucoma; OG, other glaucoma; TG, total glaucoma.
*Asterisk indicates a statistically significant (p<0.004). OR, odds ratio; TTH, tension-type headache; CI, confidence interval; UA, unadjusted; AVA, all variables adjusted; AVPA, all variables plus propensity score adjusted; OAG, open-angle glaucoma; CAG, closed-angle glaucoma; OG, other glaucoma; TG, total glaucoma.
*Asterisk indicates a statistically significant (p<0.004). OR, odds ratio; TTH, tension-type headache; CI, confidence interval; UA, unadjusted; AVA, all variables adjusted; AVPA, all variables plus propensity score adjusted; OAG, open-angle glaucoma; CAG, closed-angle glaucoma; OG, other glaucoma; TG, total glaucoma.
Table 1.
Table 2.
Table 3.
Table 4.
Table 5.
Table 6.
TOP
 KHS
KHS