Articles
- Page Path
- HOME > Headache Pain Res > Volume 25(1); 2024 > Article
-
Review Article
Application and Effectiveness of Dietary Therapies for Pediatric Migraine -
Ji-Hoon Na

-
Headache and Pain Research 2024;25(1):34-41.
DOI: https://doi.org/10.62087/hpr.2024.0007
Published online: April 17, 2024
Department of Pediatrics, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea
- Correspondence: Ji-Hoon Na, M.D., Ph.D. Department of Pediatrics, Gangnam Severance Hospital, Yonsei University College of Medicine, 211 Eonju-ro, Gangnam-gu, Seoul 06273, Republic of Korea Tel: +82-2-2019-3354, Fax: +82-2-2019-4881, E-mail: JHNAMD83@yuhs.ac
© 2024 The Korean Headache Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 8,096 Views
- 85 Download
- 7 Crossref
Abstract
- Migraine is a representative type of primary headache and a common chronic neurological disease that accounts for a large proportion of headaches in children, adolescents, and adults. Unlike migraine in adulthood, pediatric migraine occurs when brain development is not yet complete. This characteristic may require a new perspective for the treatment and management of pediatric migraine. Dietary therapies, mainly the ketogenic diet and its variants, can have positive effects on pediatric migraine. Several recent studies have revealed that dietary therapies, such as the classic ketogenic diet, modified Atkins diet, and low glycemic index diet, improve various neurological diseases by improving dysbiosis of microbiota, reducing proinflammatory cytokines, and increasing mitochondrial function. Nonetheless, the mechanism through which active dietary therapy affects pediatric migraine requires further research. To achieve this, an important role is played by the neuro-nutritional team, which can develop and manage tolerable diets for pediatric migraine patients through mutual collaboration among pediatric neurologists, nurses, and nutritionists.
INTRODUCTION
TREATMENT OF PEDIATRIC MIGRAINE
TYPES OF DIET THERAPY FOR PEDIATRIC MIGRAINE MANAGEMENT
MECHANISM OF DIET THERAPY FOR PEDIATRIC MIGRAINE
CURRENT STUDIES ON DIET THERAPY FOR PEDIATRIC MIGRAINE
CONCLUSION
AVAILABILITY OF DATA AND MATERIAL
Not applicable.
AUTHOR CONTRIBUTIONS
Conceptualization, Data curation, Formal analysis, Funding acquisition, Resources, Validation, Writing–original draft, Writing–review & editing: JHN.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING STATEMENT
This project was conducted with financial support from the Korean Headache Society.
ACKNOWLEDGMENTS
The author is grateful to all staff members and doctors in this study.
| Study | Target patient (n) | Age (yr) | Study design | Type of diet therapy | Duration of study | Outcome |
|---|---|---|---|---|---|---|
| Di Lorenzo et al.35 | 35 | 18–65 | Prospective | VLCKD | 4 wk | VLCKD patients experienced –3.73 (95% CI, –5.31 to –2.15) migraine days. |
| The 50% responder rate for migraine days was 74.28% (26/35 patients) during the VLCKD period. | ||||||
| Valente et al.15 | 23 | 47.22±15.21 | Retrospective | VLCKD, KD 2:1, MAD, LGIT | 3 mo | Reduction in monthly headache days (12.5±9.5 vs. 6.7±8.6; p<0.001) |
| Reduction in days of acute medication intake (11.06±9.37 vs. 4.93±7.99; p=0.008) | ||||||
| Reduction in patients’ weight (73.8±15.2 vs. 68.4±14.6; p<0.001) and BMI (26.9±6.2 vs. 23.7±8.1; p<0.001) | ||||||
| Tereshko et al.27 | 76 | 45.90±14.77 | Prospective | KD 2:1, LGIT, VLCKD | 3 mo | The 50% responder rate for migraine days was 74.28% (26/35 patients) during the VLCKD period. |
| KD protocols effectively improved migraine intensity, frequency, MIDAS, and HIT-6. | ||||||
| Lelleck et al.24 | First study=49 | First study=41±9.2 | Prospective | LGIT | 16 wk | Reduction of headache and migraine days, as well as reductions in HIT-6 and MIDAS scores. |
| Second study=71 | Second study=40±12.3 | Migraine days decreased by 2.40 days (95% CI, –3.37 to –1.42), HIT-6 improved by 3.17 points (95% CI, –4.63 to –1.70), and MIDAS by 13.45 points (95% CI, –22.01 to –4.89). | ||||
| Pasca et al.37 | 7 | 14–18 | Prospective | Classic KD | 3 mo | 5/7 patients reported an improvement in migraine symptoms in terms of duration of the attacks, frequency, and intensity. |
- 1. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018;38:1-211.ArticlePDF
- 2. Onofri A, Pensato U, Rosignoli C, et al. Primary headache epidemiology in children and adolescents: a systematic review and meta-analysis. J Headache Pain 2023;24:8.ArticlePubMedPMCPDF
- 3. Hershey AD. Current approaches to the diagnosis and management of paediatric migraine. Lancet Neurol 2010;9:190-204.ArticlePubMed
- 4. Alqahtani M, Barmherzig R, Lagman-Bartolome AM. Approach to pediatric intractable migraine. Curr Neurol Neurosci Rep 2021;21:38.ArticlePubMedPDF
- 5. Qubty W, Patniyot I. Migraine pathophysiology. Pediatr Neurol 2020;107:1-6.ArticlePubMed
- 6. Ackley E, Clementi MA, Yonker ME. Headache and sleep disturbances in the pediatric population. Semin Pediatr Neurol 2021;40:100924.ArticlePubMed
- 7. Powers SW, Coffey CS, Chamberlin LA, et al. Trial of amitriptyline, topiramate, and placebo for pediatric migraine. N Engl J Med 2017;376:115-124.ArticlePubMedPMC
- 8. Marshall A, Lindsay R, Clementi MA, Gelfand AA, Orr SL. Outpatient approach to resistant and refractory migraine in children and adolescents: a narrative review. Curr Neurol Neurosci Rep 2022;22:611-624.ArticlePubMedPDF
- 9. Szperka CL, VanderPluym J, Orr SL, et al. Recommendations on the use of anti-CGRP monoclonal antibodies in children and adolescents. Headache 2018;58:1658-1669.ArticlePubMedPMCPDF
- 10. Fisher E, Law E, Dudeney J, Palermo TM, Stewart G, Eccleston C. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev 2018;9:CD003968.ArticlePubMedPMC
- 11. Hindiyeh NA, Zhang N, Farrar M, Banerjee P, Lombard L, Aurora SK. The role of diet and nutrition in migraine triggers and treatment: a systematic literature review. Headache 2020;60:1300-1316.ArticlePubMedPMCPDF
- 12. Arzani M, Jahromi SR, Ghorbani Z, et al. Gut-brain axis and migraine headache: a comprehensive review. J Headache Pain 2020;21:15.ArticlePubMedPMCPDF
- 13. Papetti L, Moavero R, Ferilli MAN, et al. Truths and myths in pediatric migraine and nutrition. Nutrients 2021;13:2714.ArticlePubMedPMC
- 14. Moskatel LS, Zhang N. Migraine and diet: updates in understanding. Curr Neurol Neurosci Rep 2022;22:327-334.ArticlePubMedPDF
- 15. Valente M, Garbo R, Filippi F, et al. Migraine prevention through ketogenic diet: more than body mass composition changes. J Clin Med 2022;11:4946.ArticlePubMedPMC
- 16. Liu J, Xi K, Zhang L, Han M, Wang Q, Liu X. Tryptophan metabolites and gut microbiota play an important role in pediatric migraine diagnosis. J Headache Pain 2024;25:2.ArticlePubMedPMCPDF
- 17. McDonald TJW, Cervenka MC. Ketogenic diets for adult neurological disorders. Neurotherapeutics 2018;15:1018-1031.ArticlePubMedPMCPDF
- 18. Rezaei S, Abdurahman AA, Saghazadeh A, Badv RS, Mahmoudi M. Short-term and long-term efficacy of classical ketogenic diet and modified Atkins diet in children and adolescents with epilepsy: a systematic review and meta-analysis. Nutr Neurosci 2019;22:317-334.ArticlePubMed
- 19. Devi N, Madaan P, Kandoth N, Bansal D, Sahu JK. Efficacy and safety of dietary therapies for childhood drug-resistant epilepsy: a systematic review and network meta-analysis. JAMA Pediatr 2023;177:258-266.ArticlePubMedPMC
- 20. Di Lorenzo C, Ballerini G, Barbanti P, et al. Applications of ketogenic diets in patients with headache: clinical recommendations. Nutrients 2021;13:2307.ArticlePubMedPMC
- 21. Kossoff EH, McGrogan JR, Bluml RM, Pillas DJ, Rubenstein JE, Vining EP. A modified Atkins diet is effective for the treatment of intractable pediatric epilepsy. Epilepsia 2006;47:421-424.ArticlePubMed
- 22. Pfeifer HH, Thiele EA. Low-glycemic-index treatment: a liberalized ketogenic diet for treatment of intractable epilepsy. Neurology 2005;65:1810-1812.ArticlePubMed
- 23. Taha AY, Burnham WM, Auvin S. Polyunsaturated fatty acids and epilepsy. Epilepsia 2010;51:1348-1358.ArticlePubMed
- 24. Lelleck VV, Schulz F, Witt O, et al. A digital therapeutic allowing a personalized low-glycemic nutrition for the prophylaxis of migraine: real world data from two prospective studies. Nutrients 2022;14:2927.ArticlePubMedPMC
- 25. Schröder T, Kühn G, Kordowski A, et al. A digital health application allowing a personalized low-glycemic nutrition for the prophylaxis of migraine: proof-of-concept data from a retrospective cohort study. J Clin Med 2022;11:1117.ArticlePubMedPMC
- 26. Tereshko Y, Dal Bello S, Di Lorenzo C, et al. 2:1 ketogenic diet and low-glycemic-index diet for the treatment of chronic and episodic migraine: a single-center real-life retrospective study. J Headache Pain 2023;24:95.ArticlePubMedPMCPDF
- 27. Tereshko Y, Dal Bello S, Di Lorenzo C, et al. The effect of three different ketogenic diet protocols on migraine and fatigue in chronic and high-frequency episodic migraine: a pilot study. Nutrients 2023;15:4334.ArticlePubMedPMC
- 28. Gross EC, Klement RJ, Schoenen J, D’Agostino DP, Fischer D. Potential protective mechanisms of ketone bodies in migraine prevention. Nutrients 2019;11:811.ArticlePubMedPMC
- 29. Fila M, Chojnacki J, Sobczuk P, Chojnacki C, Blasiak J. Nutrition and calcitonin gene related peptide (CGRP) in migraine. Nutrients 2023;15:289.ArticlePubMedPMC
- 30. Fila M, Pawłowska E, Blasiak J. Mitochondria in migraine pathophysiology - does epigenetics play a role? Arch Med Sci 2019;15:944-956.ArticlePubMedPMC
- 31. Lovati C, d’Alessandro CM, Ventura SD, Muzio F, Pantoni L. Ketogenic diet in refractory migraine: possible efficacy and role of ketone bodies: a pilot experience. Neurol Sci 2022;43:6479-6485.ArticlePubMedPDF
- 32. Kilinc YB, Kilinc E, Danis A, et al. Mitochondrial metabolism related markers GDF-15, FGF-21, and HIF-1α are elevated in pediatric migraine attacks. Headache 2023;63:1076-1086.ArticlePubMed
- 33. Gross EC, Putananickal N, Orsini AL, et al. Mitochondrial function and oxidative stress markers in higher-frequency episodic migraine. Sci Rep 2021;11:4543.ArticlePubMedPMCPDF
- 34. Kossoff EH, Huffman J, Turner Z, Gladstein J. Use of the modified Atkins diet for adolescents with chronic daily headache. Cephalalgia 2010;30:1014-1016.ArticlePubMed
- 35. Di Lorenzo C, Pinto A, Ienca R, et al. A randomized double-blind, cross-over trial of very low-calorie diet in overweight migraine patients: a possible role for ketones? Nutrients 2019;11:1742.ArticlePubMedPMC
- 36. Caminha MC, Moreira AB, Matheus FC, et al. Efficacy and tolerability of the ketogenic diet and its variations for preventing migraine in adolescents and adults: a systematic review. Nutr Rev 2022;80:1634-1647.ArticlePubMedPDF
- 37. Pasca L, Toni F, Fassio F, et al. Sleep effects of Ketogenic diet in pediatric patients with migraine: preliminary data of a prospective study. Sleep Med 2024;113:238-241.ArticlePubMed
- 38. Gazerani P. Diet and migraine: what is proven? Curr Opin Neurol 2023;36:615-621.ArticlePubMed
- 39. Seng EK, Martin PR, Houle TT. Lifestyle factors and migraine. Lancet Neurol 2022;21:911-921.ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Recent Advances in the Pathogenesis and Treatment of Pediatric Migraine
家骏 马
Advances in Clinical Medicine.2026; 16(01): 1127. CrossRef - Episodic Migraine in the Pediatric Population: Behavioral Therapies and other Non-Pharmacological Treatment Options
Parisa Gazerani
Current Pain and Headache Reports.2025;[Epub] CrossRef - Current Trends in Pediatric Migraine: Clinical Insights and Therapeutic Strategies
Adnan Khan, Sufang Liu, Feng Tao
Brain Sciences.2025; 15(3): 280. CrossRef - Clinical Efficacy and Safety of the Ketogenic Diet in Patients with Genetic Confirmation of Drug-Resistant Epilepsy
Ji-Hoon Na, Hyunjoo Lee, Young-Mock Lee
Nutrients.2025; 17(6): 979. CrossRef - Clinical profile and treatment outcomes of idiopathic intracranial hypertension: a multicenter study from Korea
Kyung-Hee Cho, Seol-Hee Baek, Sung-Hee Kim, Byung-Su Kim, Jong-Hee Sohn, Min Kyung Chu, Mi-Kyoung Kang, Hee Jung Mo, Sang-Hwa Lee, Hong-Kyun Park, Soohyun Cho, Sun-Young Oh, Jong-Geun Seo, Wonwoo Lee, Ju-Young Lee, Mi Ji Lee, Soo-Jin Cho
The Journal of Headache and Pain.2024;[Epub] CrossRef - Nutritional Approaches to Managing Pediatric Migraine
Hye Eun Kwon
Headache and Pain Research.2024; 25(2): 75. CrossRef - Reduction of neck pain severity in patients with medication-overuse headache
Yooha Hong, Hong-Kyun Park, Mi-Kyoung Kang, Sun-Young Oh, Jin-Ju Kang, Heui-Soo Moon, Tae-Jin Song, Mi Ji Lee, Min Kyung Chu, Soo-Jin Cho
The Journal of Headache and Pain.2024;[Epub] CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
- Related articles
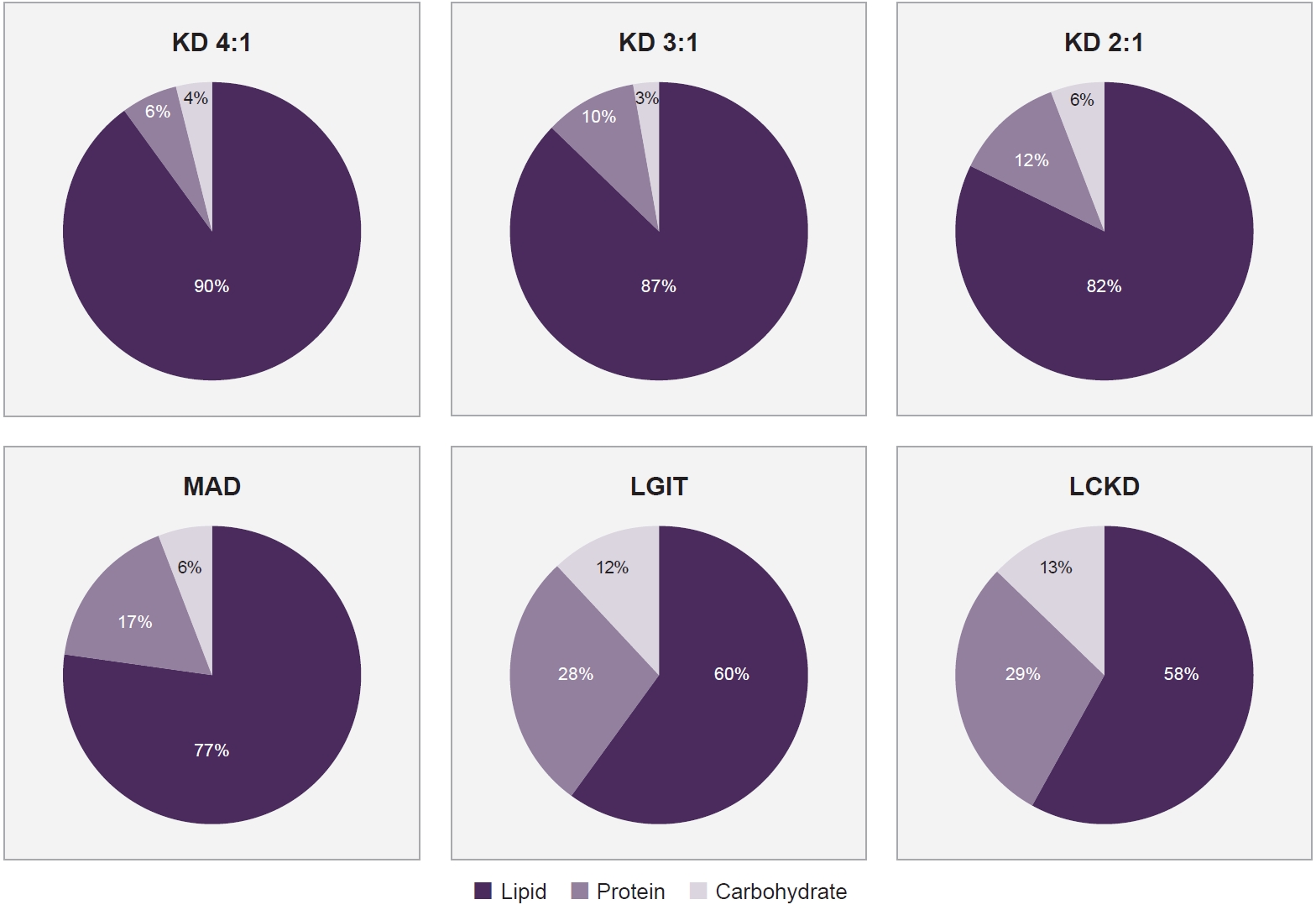
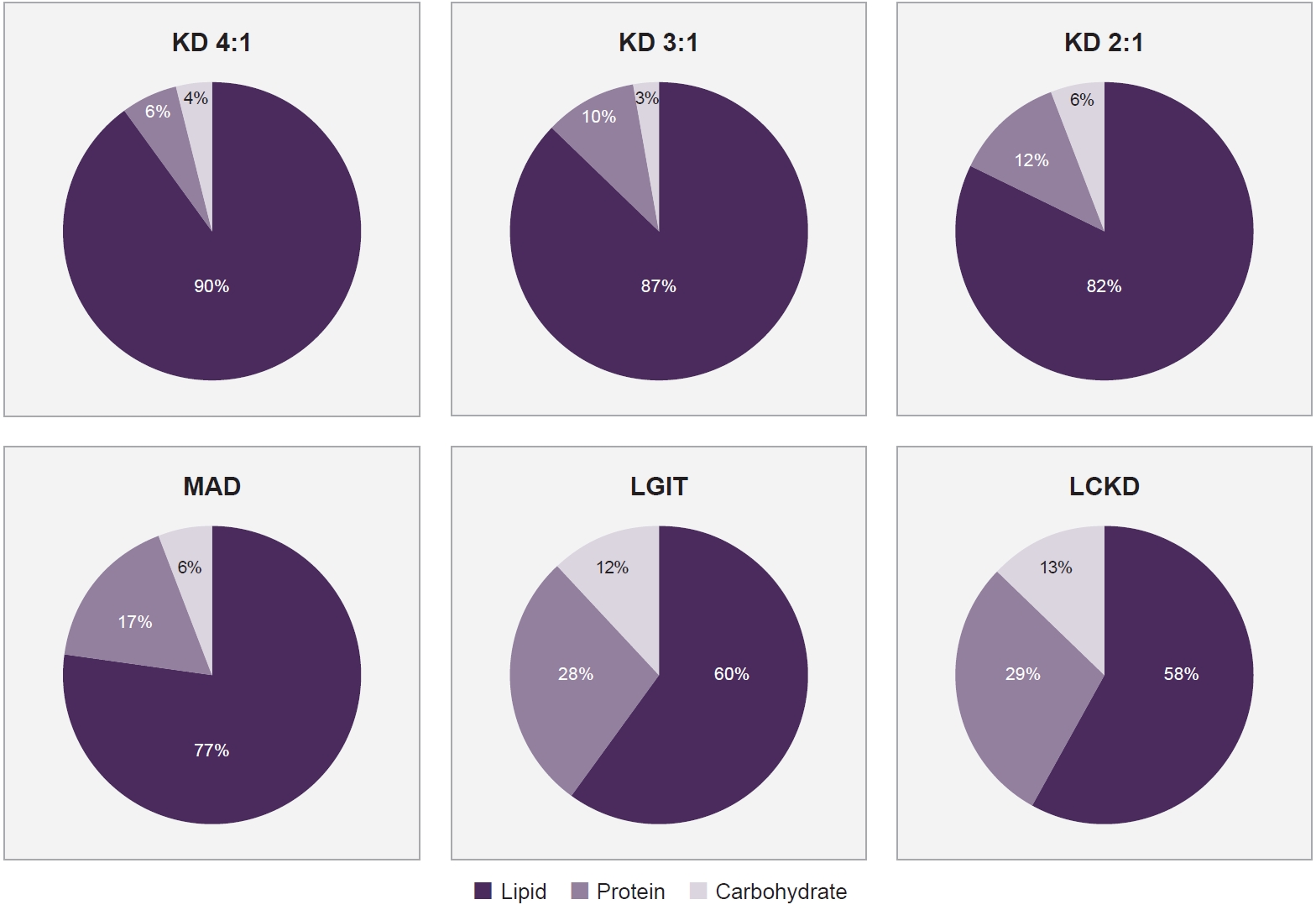
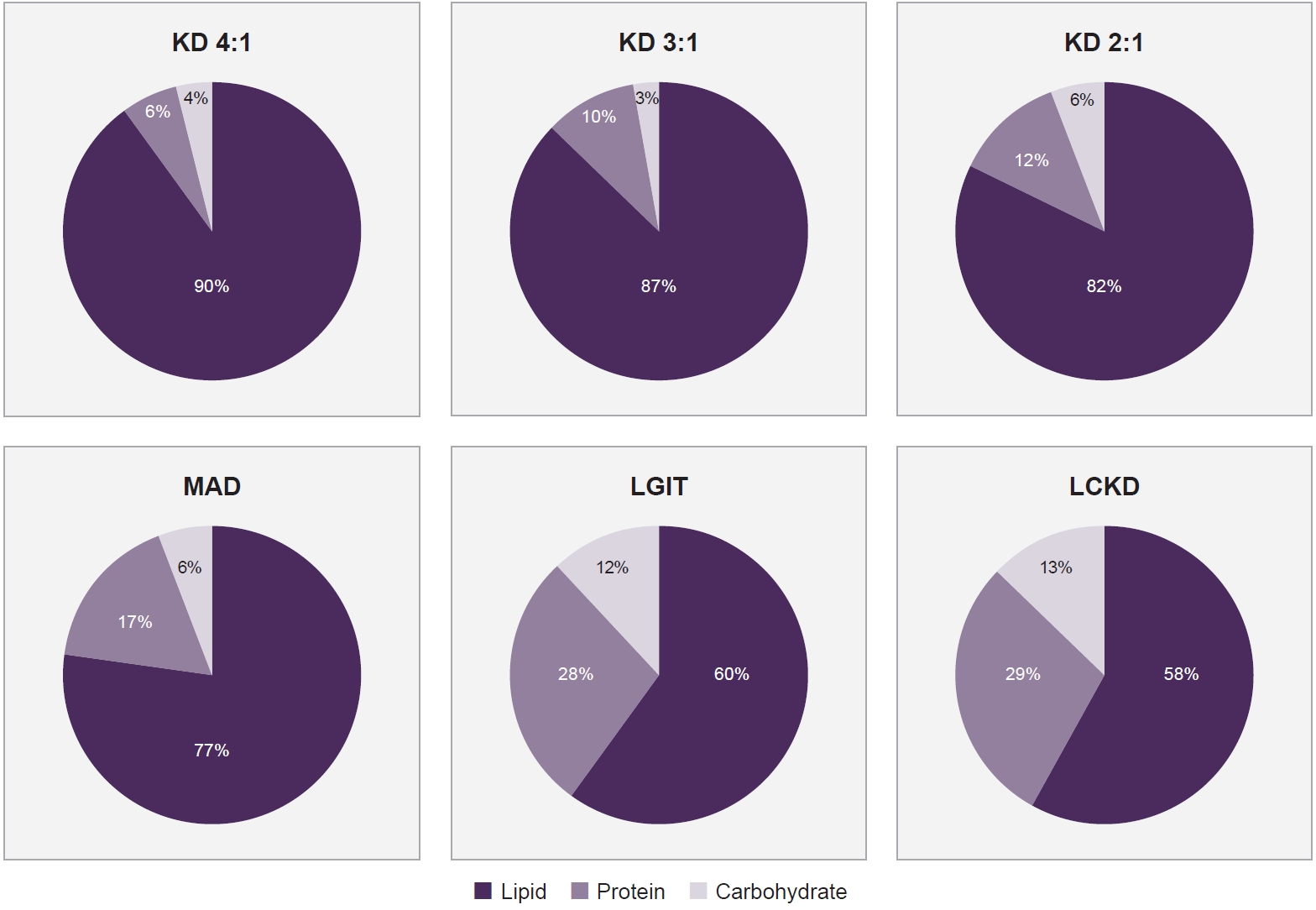
Figure 1.
| Study | Target patient (n) | Age (yr) | Study design | Type of diet therapy | Duration of study | Outcome |
|---|---|---|---|---|---|---|
| Di Lorenzo et al.35 | 35 | 18–65 | Prospective | VLCKD | 4 wk | VLCKD patients experienced –3.73 (95% CI, –5.31 to –2.15) migraine days. |
| The 50% responder rate for migraine days was 74.28% (26/35 patients) during the VLCKD period. | ||||||
| Valente et al.15 | 23 | 47.22±15.21 | Retrospective | VLCKD, KD 2:1, MAD, LGIT | 3 mo | Reduction in monthly headache days (12.5±9.5 vs. 6.7±8.6; p<0.001) |
| Reduction in days of acute medication intake (11.06±9.37 vs. 4.93±7.99; p=0.008) | ||||||
| Reduction in patients’ weight (73.8±15.2 vs. 68.4±14.6; p<0.001) and BMI (26.9±6.2 vs. 23.7±8.1; p<0.001) | ||||||
| Tereshko et al.27 | 76 | 45.90±14.77 | Prospective | KD 2:1, LGIT, VLCKD | 3 mo | The 50% responder rate for migraine days was 74.28% (26/35 patients) during the VLCKD period. |
| KD protocols effectively improved migraine intensity, frequency, MIDAS, and HIT-6. | ||||||
| Lelleck et al.24 | First study=49 | First study=41±9.2 | Prospective | LGIT | 16 wk | Reduction of headache and migraine days, as well as reductions in HIT-6 and MIDAS scores. |
| Second study=71 | Second study=40±12.3 | Migraine days decreased by 2.40 days (95% CI, –3.37 to –1.42), HIT-6 improved by 3.17 points (95% CI, –4.63 to –1.70), and MIDAS by 13.45 points (95% CI, –22.01 to –4.89). | ||||
| Pasca et al.37 | 7 | 14–18 | Prospective | Classic KD | 3 mo | 5/7 patients reported an improvement in migraine symptoms in terms of duration of the attacks, frequency, and intensity. |
VLCKD, very-low-calorie ketogenic diet; CI, confidence interval; KD, ketogenic diet; MAD, modified Atkins diet; LGIT, low glycemic index diet; BMI, body mass index; MIDAS, Migraine Disability Assessment Test; HIT-6, Headache Impact Test 6.
Table 1.
TOP
 KHS
KHS